M. Chris Gibbons MD, MPH, and Yahya Shaikh MD, MPH, Johns Hopkins Medical Institutions, The Federal Communication Commission, The Greystone Group, Inc.
To listen to a related webinar led by Chris Gibbons and Yahya Shaikh, click here.
Contact: Chris Gibbons, mcg@greystonehit.com.
What is the message?
Eight realities are rapidly creating opportunities for health system transformation. The authors outline a vision in which a minority of healthcare remains in hospitals, being surpassed by home-based care, geographic ecosystems, and technology-enabled Smart Care. Only those health organizations that take advantage of these realities will survive.
What is the evidence?
Assessment of current societal and healthcare sector trends, based on the experience of the authors.
Submitted: July 28, 2017; accepted after review: August 3, 2017.
Gibbons CM, Shaikh Y. 2017. A Vision of the Future: Organization and Delivery of Healthcare in the Digital Age. Health Management Policy and Innovation, Volume 2, Issue 2.
Eight Realities
Much has been said about the impact of emerging technologies on modern healthcare. Many entrepreneurs and investors alike are intent on developing disruptive innovations that significantly improve clinical workflows, enable predictive analytics, or enable wide-scale interoperability. While any of these would represent a significant medical advance, several factors suggest that healthcare may be about to experience an even more far-reaching disruption.
Consider the following eight realities.
- Shorter length of stay. It is widely understood that lengths of stay have dropped significantly for many conditions that previously required longer hospitalization (1, 2). The reasons for these declines are complex—related to economic factors, policy and regulatory forces, disease epidemiology, and practice changes. The key result is that, for many conditions, there has been a decline over the past two decades in care being provided in the hospital, and more care has been provided in home and community settings.
- Retail healthcare: Retail healthcare outlets are rapidly growing in popularity (3). They exhibit higher patient satisfaction, shorter waiting times, lower costs, and care quality that is on par or better than similar care provided in traditional healthcare settings (4). There is even some evidence that they do a better job than historic outlets of reaching medically underserved populations (5).
- Hospitals are dangerous. Hospitals are dangerous places! It has been well documented that many people who go to the hospital get sick from medical errors and illnesses they did not bring to the hospital (6). A recent study found that such hospital-acquired problems are so common that they are actually the third leading cause of death (7). Obviously, a tremendous amount of good is done within the current healthcare system, yet for most individuals these findings are hugely troubling.
- Mobile devices. Advances in the computer sciences and broadband networks are fueling a revolution in medical device innovation that is enabling large bedside and hospital-confined medical devices to become miniaturized, handheld, ingestible, wearable, mobile, and operable anywhere there is a broadband connection (8–13). In fact, some people who 20 years ago required stays in the intensive care unit (ICU) followed by lengthy hospitalizations prior to discharge are now are able to go home with small portable devices that do the work the ICU-based machines did just two decades ago (14, 15)! While development and use of these devices is still growing, these devices undoubtedly will reduce hospitalizations and lengths of stay.
- Robotics. Advances in robotics are now enabling surgeons based in one place to operate on patients located across town or across the globe (16–18). The spectrum of surgeries performed this way will increase in the future. Given the early results and global need for providers and medical assistants, these systems will continue to advance and be used.
- Telehealth. Telemedicine and telehealth have advanced rapidly. Innovations are enabling physicians to see, talk to, examine, and monitor their patients remotely, lowering the need for inconvenient visits to the doctor’s office or unnecessary visits to the ER or hospital (19–22, 22–27).
- Cost structure. Hospitals were in part developed to centralize resources in order to gain scale economies and scope opportunities (28). In the future, however, hospitals may not be able to reduce costs below that of ambulatory care delivery. Also, because of technological advances built on broadband networks, there may no longer be significant scope opportunities arising from centralization of medical infrastructure.
- Artificial intelligence. Finally, the emergence of artificial intelligence and cognitive computing is providing unprecedented levels of data tracking and analytic capacity. These innovations are generating insights that are instantly available to medical providers, patients, and caregivers (29–31).
So, Why Would Anyone Stay in a Hospital or Pay for Hospital Services?
These realities raise two questions. Why would patients, in the future, ever choose to stay in a hospital? Why would payers insist that covered beneficiaries obtain care in high-risk hospitals when lower-risk and lower-cost options with (at least) comparable outcomes and higher patient satisfaction levels are available? Healthcare systems and hospitals, as they currently exist, will face threats to their existence.
If hospitals, as we know them, do not survive, what will the hospitals and healthcare systems of the future look like? While predicting the future is fraught with challenges, it is becoming increasingly clear that those hospital systems that proactively embrace the opportunities of these realities, and innovate on the very notion of the structure and functions of a hospital, will be best able to overcome the challenges, provide value to patients, and remain financially viable.
A Vision of the Future
Several experts have described possible future organization and delivery of healthcare systems that provide useful thoughts and perspectives (32–36), but none provides a comprehensive vision that accounts for realities we have described and for the national trends that are shaping healthcare today. Key trends include, at a minimum, a recent national population surge, an increasingly aged and diverse national demographic, significant and growing healthcare provider shortages and maldistribution, a focus on both social and medical/genetic determinants of health, rising costs of care, and the role of technology. This is a daunting list of challenges.
We briefly assess future healthcare delivery in an attempt to provide a more comprehensive vision. We do not believe this or any other model is perfect, yet it provides a valuable base for discussion.
Figure 1 summarizes the major components of this vision. Briefly, there will be a continuing contraction in the volume of inpatient hospital services. This contraction is likely to be so significant that its impact will be fatal to many currently existing hospitals and result in so significant a restructuring of other hospitals that the majority that survive may bear so little resemblance to the hospitals of today, they may no longer be called hospitals.
-
Critical care remaining in hospitals: 10 percent to 15 percent
Surviving institutions will focus on patients who are of the highest acuity, critically ill, and medically complex. These patients need procedures and therapies that cannot be provided in a less controlled setting. Nonetheless, given the fact that many conditions that years ago could only be treated in intensive care units today are managed in part with technology in ambulatory and home settings, this type of hospital-based critical care will have declining demand.
Care in these facilities will be driven by physician providers, as it often is today. Unlike the healthcare systems of today, though, this type of care will likely represent the smallest proportion of the volume of care provided nationally. This volume of care at any time might be 10 to 15 percent.
-
Hospital at home: 15 percent to 25 percent
There will be other patients who could benefit from inpatient care services but otherwise do not need to be in a hospital. Due to advances in telemedicine and telehealth; mobile, wearable, embeddable, and cloud computing; plus advances in artificial intelligence and cognitive computing, lower-acuity patients will increasingly receive ambulatory care in the community or at home. Advances in broadband-enabled health technologies will further contribute to the value and cost effectiveness of ambulatory models of care. This trend is rapidly increasing.
Indeed, multiple studies are demonstrating the value and role of so-called “Hospital at Home” models of care delivery (37–42). The share of total volume for the hospital at home model of care may comprise as much as 15 to 25 percent.
-
Geographic ecosystems: 30 percent
Several companies from beyond healthcare are beginning to innovate in the healthcare sector. Examples include IBM, Microsoft, Google, Apple, and Amazon, to name a few from the tech sector. Industries as varied as automobiles (43) and residential buildings (44–45) are also exploring opportunities in the health sector. While not yet a reality, in the near future, whole residential communities, including automobiles in transit, could be sites for effective health and low-acuity medical care. Such a model of care could easily become part or even supplant the current notion of Accountable Care Organizations, in which virtual health systems are responsible for the care of people living within a region.
The new geographic ecosystems could be optimized for post-acute care and chronic disease self-management. To help keep costs down, they may be primarily directed by nurse practitioners and nurses, who oversee larger numbers of enabling services staff including patient navigators, community health workers, and Promatoras (46–50). In the future, the regional model of healthcare delivery may account for as much as 30 percent of volume.
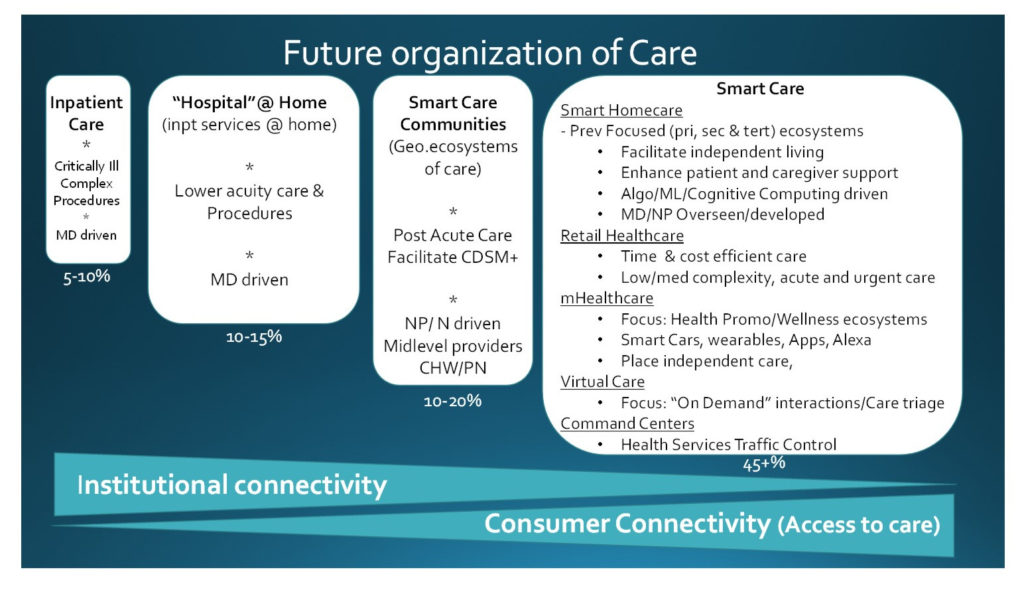
Figure 1. The Future Organization of Healthcare Delivery
-
Smart Care: 40 percent to 50 percent
Digital health and consumer health informatics are continuing to grow and evolve in society. Indeed, care delivery that is mediated at least in part through these mechanisms may well become the largest model of care delivery. This could account for as much as 40 to 50 percent of the volume of care.
We call this model Smart Care. The Smart Care term highlights the fact that advances in computer processing, data storage, and miniaturization are pushing computing power to the edges of the network. As a result, consumer devices are rapidly becoming smarter.
By becoming smarter, consumer devices will operate autonomously to detect, decide, and react to needs based on predetermined algorithms, without direct human input of a healthcare provider. Many of these solutions will not be individual hardware products, but rather be built into the walls of buildings and under the hoods of cars. Ultimately, they will be woven into the fabric of society in a way that does not require a patient’s active choice in order to capture needed information or respond appropriately. Such passive interventions have been recognized by public health and medical experts as among the most powerful health interventions possible.
Consider the health benefits of water fluoridation, iodination of salt, and airbags. In parallel, homes and automobiles could themselves become smart and integral components of a broader consumer health ecosystem that is always on, following people wherever they are. In doing so, SmartCare innovations could help individuals live independently, safely, focus on wellness and prevention, and help manage minor health issues and low-acuity medical complaints.
Who might lead the SmartCare revolution? Tech companies already see this as the next frontier. Retail healthcare organizations might also become major players in exploring and advancing this model of care delivery. So might virtual reality and augmented reality designers and innovators.
And as this model of care delivery grows there will be needs for health technology “air traffic controllers” and “control centers.” These individuals and organizations would have key responsibilities for optimizing data and information flows. They will also need to coordinate the use of human resources in the community setting.
This coordinating role is a potential opportunity for current health systems to embrace the disruptive innovations. Some large health systems are already thinking about these possibilities and preparing to act. For instance, Mercy Hospital system in St. Louis, Missouri, has developed the first operational “Hospital without beds”—focusing on optimizing care via technology at a distance to patients within its network (51).
-
Broadband: Making it all work together
Full-scale broadband connectivity—both institutionally and in the home—is central to this vision of healthcare delivery. As the two arrows at the bottom of the graphic illustrate, if we focus only on institutional connectivity, some consumers may have little or no access to services. If, instead, we also prioritize consumer access to broadband connectivity, all consumers will have access to at least some forms of effective healthcare goods and services.
Conclusions
We have presented a vision of future healthcare organization and delivery that considers major forces bringing change not only to medical systems, but to society. This model envisions both a restructuring of the traditional healthcare system and a transformation in what is defined as healthcare. The new definition includes traditional forms of in-person healthcare, but in addition also includes many types of technologically mediated health interactions, some of which do not involve a human provider, plus other forms of technology-based care that focuses on patient behaviorism, wellness, and prevention. These shifts will inevitably broaden the definition of what is considered “healthcare.” With large tech companies making serious forays into healthcare, and the technological components and data derived from their devices becoming ever more powerful at the point of need both for patients and their providers, the lines of distinction between healthcare organizations and at least some technology companies will blur. This will have tremendous implications on healthcare costs, payments, reimbursement, and even insurance.
The changes will likely also mean there will be a shift in who is defined as a “provider.” As technologies evolve to enable increasing degrees of support for consumers and their families, formal and informal out-of-hospital caregivers will assume greater importance in providing solutions. The solutions themselves will increasingly be tailored to both patients and their caregivers.
Finally, where healthcare happens likely will undergo the most significant change. While important aspects of healthcare will still be provided in the institutional setting, considerably more care will be provided in the ambulatory, community, and home settings. In addition, with the coming advances in 5G broadband and its widespread availability, at least some forms of healthcare will increasingly happen on demand, day or night, whenever the patient wants or needs it, wherever the patient is located.
Of course, there are many barriers to achieving this vision. However, we believe that the cat is already out of the proverbial bag. Already, we are well on our way to a transformation that, in whole or in part, will reflect the vision we describe.
Like it or not, the future of healthcare will not likely be controlled by the current healthcare sector, insurance providers, or the federal government. Given the traditional incremental nature of change that is common in medical care and policy, the role of these entities will increasingly be ancillary and reactive. Instead, consumer demands, market realities, and business opportunities will likely profoundly shape the future healthcare delivery system. Ultimately, only those health organizations that recognize and take advantage of these realities will survive.
References
- Mardis R, Brownson K. Length of stay at an all-time low. Health Care Management. 2003; 22(2): 122-7.
- DeFrances CJ, Hall MJ. 2005 National Hospital Discharge Survey. Advance Data. 2005;12(385):1-19.
- Mehrotra A, Lave JR. Visits to retail clinics grew fourfold from 2007 to 2009, although their share of overall outpatient visits remains low. Health Affairs. 2012; 31(9): 2123-9.
- Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for three common illnesses. Annals of Internal Medicine. 2009; 151(5): 321-8.
- Mehrotra A, Wang MC, Lave JR, et al. Retail clinics, primary care physicians, and emergency departments: a comparison of patients’ visits. Health Affairs. 2008; 27(5): 1272-82.
- Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Affairs. 2011; 30(4):596-603.
- Makary MA, Daniel M. 2016. Medical error-the third leading cause of death in the US. British Medical Journal; 2016; 353: 2139.
- Gibbons MC, Wilson RF, Samal L, et al. Consumer health informatics: results of a systematic evidence review and evidence based recommendations. Translational Behavioral Medicine. 2011; 1(1):72-82.
- Gibbons MC. A historical overview of health disparities and the potential of eHealth solutions. Journal of Medical Internetational Research. 2005; 7(5):e50.
- Health IT. What is telehealth? How is telehealth different from telemedicine? 2014. https://www healthit gov/providers-professionals/faqs/what-telehealth-how-telehealth-different-telemedicine. Updated January 9, 2017. Accessed March 1, 2017
- Finkelstein J, Knight A, Marinopoulos S, et al. Enabling patient-centered care through health information technology. Evidence in Replicating Technology Assessment. 2012; June:1531.
- Yilmaz T, Foster R, Hao Y. Detecting vital signs with wearable wireless sensors. Sensors. 2010; 0(12):10837-62.
- Darwish A, Hassanien AE. Wearable and implantable wireless sensor network solutions for healthcare monitoring. Sensors. 2011; 11(6):5561-95.
- Kiourti A, Nikita KS. A review of in-body biotelemetry devices: implantables, ingestibles, and injectables. IEEE Transactions in Biomedical Engineering. 2017; 64(7):1422-30.
- Kiourti A, Psathas KA, Nikita KS. Implantable and ingestible medical devices with wireless telemetry functionalities: a review of current status and challenges. Bioelectromagnetics. 2014; 35(1):1-15.
- Hussain A, Malik A, Halim MU, et al. 2014. The use of robotics in surgery: a review. International Journal of Clinical Practice. 2014; 68(11):1376-82.
- Avgousti S, Christoforou EG, Panayides AS, et al. Medical telerobotic systems: current status and future trends. Biomedical Engineering Online. 2016; 15(1):96.
- Ballantyne GH. Robotic surgery, telerobotic surgery, telepresence, and telementoring: Review of early clinical results. Surgical Endoscopy. 2002; 16(10):1389-402.
- Catarinella FS, Bos WH. Digital health assessment in rheumatology: current and future possibilities. Clinical Experimental Rheumatology. 2016; 34(5), Suppl (101):S2-S4.
- Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Affairs. 2014; 33(2):194-9.
- Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Internaltional Journal of Medical Informatics. 2010; 79(11): 736-71.
- Khan N, Marvel FA, Wang J, Martin SS. Digital health technologies to promote lifestyle change and adherence. Currernt Treatment Options in Cardiovascular Medicine. 2017; 19(8):60.
- Hollis C, Falconer CJ, Martin JL, et al. Annual research review: digital health interventions for children and young people with mental health problems—a systematic and meta-review. Journal of Child Psychology and Psychiatry. 2017; 58(4):474-503.
- Bhattarai P, Phillips JL. The role of digital health technologies in management of pain in older people: an integrative review. Archives of Gerontology and Geriatrics. 2017; 68:14-24.
- Kaufman N, Khurana I. Using digital health technology to prevent and treat diabetes. Diabetes Technology and Therapy. 2016; 18, Suppl 1:S56-S68.
- Widmer RJ, Collins NM, Collins CS, et al. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clinic Proceedings. 2015; 90(4):469-80.
- Thomas JG, Bond DS. Review of innovations in digital health technology to promote weight control. Current Diabetes Reports. 2014; 14(5):485.
- Starr P. 1982. The Social Transformation of American Medicine. New York: Basic Books; 1982.
- Chen Y, Elenee Argentinis JD, Weber G. IBM Watson: how cognitive computing can be applied to big data challenges in life sciences research. Clinical Therapy. 2016; 38(4):688-701.
- Wu H, Yamaguchi A. Semantic web technologies for the big data in life sciences. Bioscience Trends. 2014; 8(4):192-201.
- Martin-Sanchez F, Verspoor K. Big data in medicine is driving big changes. Yearbook of Medical Informatics. 2014; 9:14-20.
- Charlesworth K, Jamieson M, Butler CD, et al. The future healthcare?. Australian Health Review. 2015; 39(4):444-7.
- Nagle LM, Pitts BM. Citizen perspectives on the future of healthcare. Healthcare Quarterly. 2012; 15(2):40-5.
- Mezghani E, Da SM, Pruski C, et al. A perspective of adaptation in healthcare. Studies in Healthcare Technology Informatics. 2014; 14(205):206-10.
- Sklar DP. Delivery system reform—visualizing the future. Academic Medicine. 2013; 88(7):905-6.
- Kimball B, Joynt J, Cherner D, et al. The quest for new innovative care delivery models. Journal of Nursing Administration. 2007; 37(9):392-8.
- Wilson A, Parker H, Wynn A, et al. Performance of hospital-at-home after a randomised controlled trial. Journal of Health Services Research and Policy. 2003; 8(3):160-4.
- Wilson A, Wynn A, Parker H. Patient and carer satisfaction with “hospital at home”: quantitative and qualitative results from a randomised controlled trial. British Journal of General Practice. 2002; 52(474):9-13.
- Jones J, Wilson A, Parker H, et al. Economic evaluation of hospital at home versus hospital care: cost minimisation analysis of data from randomised controlled trial. British Medical Journal. 1999; 319(7224):1547-50.
- Wilson A, Parker H, Wynn A, et al. Randomised controlled trial of effectiveness of Leicester hospital at home scheme compared with hospital care. British Medical Journal. 1999; 319(7224):1542-6.
- Richards SH, Coast J, Gunnell DJ, et al. Randomised controlled trial comparing effectiveness and acceptability of an early discharge, hospital at home scheme with acute hospital care. British Medical Journal. 1998; 316(7147):1796-801.
- Shepperd S, Harwood D, Gray A, et al. Randomised controlled trial comparing hospital at home care with inpatient hospital care. II: cost minimisation analysis. British Medical Journal. 1998; 316(7147):1791-6.
- Stoaks U. The next big digital health platform for entrepreneurs to build on: your car. Forbes. September 1, 2015. https://www.forbes.com/sites/unitystoakes/2015/09/01/the-next-big-digital-health-platform-for-entrepreneurs-to-build-on-your-car/#659f85db6895. Accessed March 1, 2017.
- (44) Tso R. Smart homes of the future will know us by our heartbeats. Wired. December 5, 2016. https://www.wired.com/insights/2014/10/smart-homes-of-the-future/. Accessed March 1, 2017.
- Karten S. Beyond the smart home: the health hub of the future. HIT Consultant. March 9, 2016. http://hitconsultant.net/2016/03/09/beyond-the-smart-home-the-health-hub-of-the-future/. Accessed March 1, 2017.
- Gibbons MC, Tyus NC. Systematic review of U.S.-based randomized controlled trials using community health workers. Progressive Community Health Partnerships. 2007; 1(4):371-81.
- Whiteman LN, Gibbons MC, Smith WR, et al. Top 10 things you need to know to run community health worker programs: lessons learned in the field. Southern Medical Journal. 2016; 109(9):579-82.
- Eckenrode J, Campa MI, Morris PA, et al. The prevention of child maltreatment through the nurse family partnership program: mediating effects in a long-term follow-up study. Child Maltreatment. 2017; 22(2):92-9.
- Olds DL, Robinson J, Pettitt L, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics. 2004; 114(6):1560-8.
- Olds DL, Robinson J, O’Brien R, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002; 110(3):486-96.
- Pepitone J. The $54 million hospital without any beds. http://money.cnn com/2016/09/12/technology/mercy-hospital-virtual-care/index html. Updated September 12, 2016. Accessed March 3. 2017.
