David A. Lubarsky; Steven G. Ullmann; John Tawwater; Myka B Whitman; Melissa Black; Kaming Lo; Shari Messinger Cayetano; Lisa F Rosen; David J Birnbach
Contact: David A. Lubarsky, dlubarsky@med.miami.edu
Disclosures: No funding was received in relation to this study. None of the authors declare any conflicts of interest.
Abstract
What is the message?
The study found that when a large physician group at a public hospital received sovereign immunity (SI) from malpractice litigation, the incidence of serious harm decreased over time and the implementation of SI did not impact the safety of care delivered.
What is the evidence?
To explore the impact of tort reform on adverse events, the incidence of serious patient harm was evaluated over a six-year period where care was provided by a single, large physician group. At Jackson Memorial Hospital, a public hospital, physicians were protected from large medical malpractice claims by sovereign immunity for the last four years of the six-year study.
Submitted: November 16, 2017. Accepted after review: December 20, 2017
Cite as: David A. Lubarsky, Steven G. Ullmann, John Tawwater, Myka B Whitman, Melissa Black, Kaming Lo, Shari Messinger Cayetano, Lisa F Rosen, David J Birnbach. The impact on the rate of adverse events after granting private physicians sovereign immunity at a public hospital. Health Management Policy and Innovation, Volume 3, Issue 1.
Introduction
With the ongoing concern about quality and safety1, healthcare providers are focused on reducing adverse events and creating the best systems to improve outcomes2. Significant initiatives to impact practice include data sharing3, education and debriefings4, safety management systems5, electronic medical records6,7, checklists and time-outs8-10, leadership and accountability11, and error reporting2. However, the plaintiff’s bar continues to believe that there is a role that the tort system plays in monitoring physician’s behavior and providing a check on healthcare systems that might otherwise lack sufficient oversight for optimal safety12.
Trial attorneys have been forceful in publicizing medical errors as a legitimate way to alert the public to deficiencies in proper care, and they claim that litigation motivates providers to practice more safely13 and maintain a high quality of care14,15. Published reports agree that improvements in patient safety lead to better practices and reduced malpractice claims16. On the other hand, there is conflicting evidence whether defensive medicine or malpractice suits improve quality of care17-19. For example, there are inconsistent findings as to the impact of malpractice suits may on the rate of Caesarean-sections in obstetric practices13,20.
The threat of lawsuits has a major impact, and is driving current governmental efforts at tort reform. In many areas of the United States, rising medical malpractice premiums have become unmanageable; furthermore, the economic and social costs of malpractice claims may drive physicians away from specialties and environments that are considered high risk21-23. Additionally, the fear of lawsuits may lead to the practice of defensive medicine—the unnecessary ordering of tests and services to reduce a physician’s liability costing nearly $50 billion annually24-28.
Background
In 1952, an agreement designated Jackson Memorial Hospital (JMH) as the teaching hospital for the University of Miami Miller School of Medicine. This arrangement stipulated that Miami-Dade County would operate JMH for both the indigent and for patients who could pay. The University of Miami, through the School of Medicine, provided the faculty to care for the patients and train residents. (Figure 1) What this meant, in fact, is that while JMH was protected by sovereign immunity (SI) as a government entity, the individual physicians who worked for the University of Miami could be held liable for medical errors. As a result, this exposed the University physicians as the only “deep pockets” during the care of South Florida’s most difficult and complex cases. Recognizing the importance of public teaching hospitals, resident education and resident retention throughout the State of Florida, and the disproportionate share of liability imposed on private medical school in Florida that provide patient care at public teaching hospitals, in 2011, the State of Florida extended the protections of sovereign immunity to any private medical school in Florida (including its physicians and employees) that had a contractual agreement with a public teaching hospital to provide patient care serves at such hospitals. As a result of this amendment, the University of Miami and JMH amended their long-standing contractual relationship so that the 900 clinically active employed physicians at the University of Miami could be deemed agents of JMH and received the protections of sovereign immunity when they were providing medical care at a JMH facility. The same 900 clinically active employed physicians were on staff at the University’s privately-owned, 560 bed, University of Miami Hospital (UMH) and continued to practice there without SI.
Study Aims
This unique setting allowed us to evaluate the temporal trends on safety events without tort reform and to isolate the impact of tort reform on the same physicians practicing at JMH who had received SI. There has never been a recorded instance of disparate tort application in such close proximity at two hospitals, let alone for the same physician group; usually comparisons only exist over time and/or across different state borders. Nor has any research previously been conducted to evaluate safety events related to SI over such a prolonged time period using objective auditable safety data from a large single physician group. In planning the study, we wanted verify that if the rate of serious events did not increase, it was not an anomaly. To achieve this, we used UMH as a control hospital to assess the natural rate of change in safety events over time for the same physicians. Given this opportunity to assess the impact of the threat of malpractice on patient safety events, we hypothesized there would be no impact from the granting of tort reform protections and that the incidence of harmful events would not increase at JMH.
Methods
Quantros, a provider of software that collects and quantifies safety data, provided report summaries with graded harm were available from 2010 to 2015 at JMH and also at the comparator hospital UMH. Only two years pre-SI were collected using this software, thus limiting the data set for the pre-SI years. Serious harm was defined as category G =Event may have contributed or resulted in permanent harm; H=Event that required intervention to sustain life; and I=Death related to event or cause unknown. Annual safety outcomes were defined as the log of the incidence of serious harm reports/patient bed days, adjusting for volume of care. SAS version 9.4 was used to analyze the data.
Total unique number of claims, total dollar value of claims, and average dollar value of claims involving UM attending physicians at JMH were evaluated for 2010-2011 versus the 2012-2013 time periods. The analysis extended only to 12/31/2013 to account for the expiration of the two-year statute of limitations which would assure an examination of a virtually complete set of malpractice claims that could be filed. Any open claims from those time periods that had not been settled were valued at the reserves set by the legal team (at the likely settlement value).
Statistical analysis: The appendix to the paper describes the statistical analysis that we undertook with the data.
Results
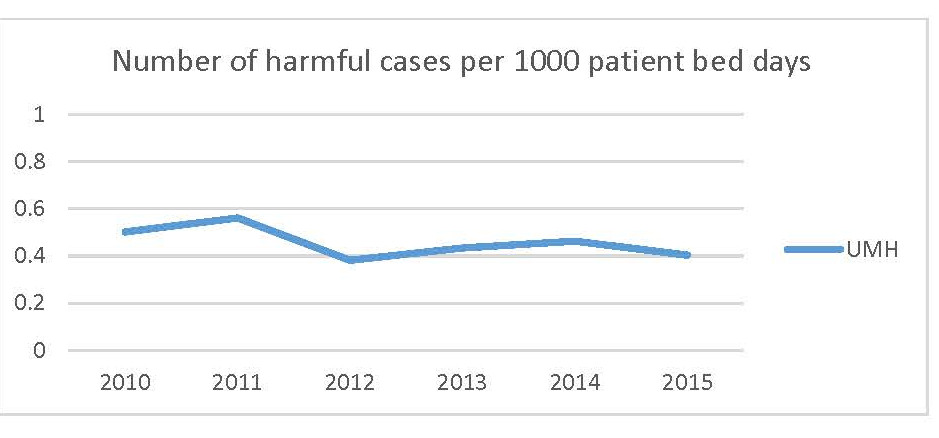
At JMH, where University of Miami physicians received SI, the incidence of harmful events declined significantly after SI comparing the pre vs post period. The post-SI average incidence rate of harmful event among the four post-SI years was 13% lower (estimate=-0.1368, RR=0.8721, p=0.0109) compared to the two pre-SI years (Table 1). The trajectory of changes in the incidence of harmful events over time was not significantly different at UMH versus JMH (with SI) (Figure 2B). The case mix index (CMI), a measure of severity of patient presentation, increased slightly over time at both hospitals (Table 2). Over the period of the study, the university faculty practice employed approximately 900 physician clinicians reporting work relative value units. Approximately two-thirds delivered care at both hospitals during those years. For example, in the last year of the study, the exact numbers employed were 919 physicians and 66.7% delivered care at both hospitals.
There was a marked decline in the total ($16.5M vs $0.7M) and average ($3.3M vs $0.233M) dollar value of claims at JMH following SI for the university faculty practice. Despite an intention to perform a statistical analysis, there were an insufficient numbers of claims to provide a valid statistical analysis.
Discussion
The implementation of SI at JMH did not impact the safety of care delivered. In order to rule out that the safety of care was not compromised and might have been unrelated to SI, a comparison to UMH showed similar findings. Our study provides the first opportunity to assess whether the threat of significant malpractice exposure drives the safety of care delivered by physicians.
There is only one previous direct study of disparate tort protections on total quality of care25. A single hospital corporation with hospitals in Texas (TX) and Louisiana (LA) assessed CMS quality of care indicators over a common time period after caps on pain and suffering were introduced in TX but not in LA. That evaluation occurred at widely separated sites and with totally disparate medical staffs, unlike our study. Regardless, their findings were similar to ours. From 2000-2006, there was no impact of tort reform on quality of care between those who had caps on pain and suffering in Texas and hospitals owned in Louisiana by the same parent company where caps were not in place. The only difference was in the dramatic decline in malpractice cases brought in Texas based on non-economic damages.
Similarly, in our study, there was a similar marked decline in the dollar value of lawsuits brought against University of Miami physicians practicing at JMH following the granting of SI. In a second study, also consistent with our findings, a single academic surgical department reported a significant decline in the cost of malpractice following tort reforms, but no other physician group studies exist21.
There are several studies that have examined the impact of tort reform (most often non-economic caps) across statewide or national claims databases on the care of patients with coronary artery disease or labor and delivery. Several of those studies found a decline in procedural treatment intensity associated with tort reform26,29; others have shown that there is a larger impact on diagnostic intensity27. A reduction in either diagnostic or procedural activity would be expected to yield fewer possible safety errors and is consistent with our findings of reduced reports of safety events.
Since tort reform almost uniformly involves caps on pain and suffering, and in all previous cases have been implemented at the same time across an entire state, studies in the medical and legal literature have only been able to evaluate sequential performance over time without adequate control.25 These before/after studies of a tort reform intervention may not be able to fully control for changing care paradigms, nor can they control how documentation initiatives change reporting of quality over time for the physicians or facilities affected.
Our ability to control for the severity of patients treated via the trajectory of safety events occurring over time, and reporting paradigms for safety events for the same physician group by assessing these variables 250 yards away in a different tort environment, are unique and unlikely to be repeated. We were thus able to rule out impacts of the expected increased focus over time on patient safety (which was parallel in both institutions), which might otherwise confuse definitive evaluation of safety performance. We were therefore able to determine that performance of the physicians after being granted SI was better in terms of serious patient safety events and comparable to the performance over time when compared to a private hospital environment in which such protections did not exist.
This study had controls to conclude that physician behaviors related to patient safety were not impacted by the either SI or the threat of a lawsuit. The patient population did not have a reduced acuity of care that could account for the reduced safety events. At JMH, and at the comparator UMH, CMI increased, and thus one would expect more, not the same or fewer safety events based on patient severity of illness. It was controlled for volume (rate adjusted by patient bed days), temporal trending (no difference with control hospital related to a reduction in serious patient harm reporting), and geography (the two hospitals were across the street from one another). It was also controlled for physicians, since the vast majority of care in both hospitals was provided by the same group of approximately 900 physicians, assisted by 1,000 rotating residents and fellows under their supervision. In addition, leadership of all academic departments spanned both hospitals, and the patient safety administrators at both hospitals remained consistent throughout the study period.
It is important to note that we did not seek to compare the rate of safety events at UMH with JMH. The two facilities, while doing a similar number of elective surgical procedures, have a different number of licensed beds, disparate socio-economic patient populations, and unique service lines (e.g. a Level 1 trauma center, organ transplant program, obstetrics and neonatal ICU only at JMH, and technologically advanced non-invasive minimally invasive cardiology at UMH). We only compared each hospital’s own specific trajectory of serious safety events to address the potential that JMH safety event performance could have been improved over time had SI not been granted. Since the trajectories between safety events at the two hospitals were similar (both declined a similar amount over time), we can dismiss that as a limitation of the study.
Nonetheless, there are six limitations. First, a small subset of physicians only deliver care at either UMH or JMH and thus would not be affected by the initiation of SI. Since this group comprised only approximately 1/3rd of the total number of faculty, it is unlikely this impacted the overall results. Their practice patterns remained constant and were not isolated, as all of them served in academic departments overseeing practice at both institutions. Second, the impact of SI on physicians who spend more time at either hospital could not be individually evaluated; there might be a subset of physicians where SI did drive practice decisions despite the larger group demonstrating no effect. Third, rotating interns and residents change monthly, and each year a new class begins. Because the attending physician is ultimately responsible for the residents, we believe that the impact of varying identity of residents on different services would have a negligible effect over such a prolonged time period. In addition, both hospitals had new faculty hired after the initiation of SI, so it is unclear if any of these changes had a subtle influence on practice. Fourth, while we do not believe there was a failure to enter G, H, and I events in the Quantros system, this is unverifiable since all such outcomes were reported through this mechanism. The vast majority of Quantros events are entered by nursing staff, and since they were unaffected by the granting of SI, it is likely their reporting patterns remained unchanged through the study period. Fifth, University physicians, whether they received sovereign immunity or not, were protected by insurance provided by the medical group and do not directly pay for their own premiums, such as private practice physicians might, limiting the personal financial impact of sovereign immunity. However, while University physicians may not be personally liable, they may experience acute stress disorder, shame, and self-doubt, a condition now known as the ‘second victim’30. After being granted SI, and given the presence of trainees, one might imagine less oversight and management by the attendings after the threat of lawsuits was eliminated in the public hospital, but there was no evidence this occurred based on the declining incidence of serious safety events. Sixth, the practice of offensive medicine (additional highly remunerative procedures after tort reform26, and its impact on total quality of care, would not be expected in the University of Miami’s salaried academic faculty. This might have resulted in a slight decrease in the incidence of safety events compared to a fee for service population of physicians.
The results of this study suggest that norms of practice, along with a stable physician commitment to providing the best care possible, are maintained without the threat of malpractice lawsuits. Further, the persistence of safe practice patterns over at least four years following the granting of SI leads us to conclude that the threat of malpractice is not a significant driver of safe physician behaviors. A well-functioning liability system should provide incentives to institutions that adopt safer systems, since tort reform on its own does not achieve this goal25,27. These investments should result in fewer adverse events and increased quality31. We believe that physicians are inherently committed to achieving sustainable patient safety practices, and, as we expected, adhere to professional standards regardless of the threat of being sued.
Contributors: DAL jointly conceived the study with DJB and MB. CT, MW, KL, SM, LFR and MB were involved in the study design and provided collated data. All authors were involved in analysis and interpretation of the data. All authors revised it critically for important intellectual content and approved the final version. DAL is guarantor.
Funding: This study received no funding.
Ethical approval: This study was granted exemption from the university’s Institutional Review Board.
Transparency statement: The lead authors (the manuscript’s guarantors) affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
The authors gratefully acknowledge Maureen Fitzpatrick, MSN, ARNP-BC, for her assistance with the manuscript.
Note: The first paragraph in the Background section of the initial version of this article read as follows:
In 1952, an agreement designated Jackson Memorial Hospital (JMH) as the teaching hospital for the University of Miami Miller School of Medicine. This arrangement stipulated that Miami-Dade County would operate JMH for both the indigent and for patients who could pay. The University of Miami, through the School of Medicine, provided the faculty to care for the patients and train residents. (Figure 1) What this meant, in fact, is that while JMH was protected by sovereign immunity (SI) as a government entity, the individual physicians who worked for the University of Miami could be held liable for medical errors. As a result, this exposed the University physicians as the only “deep pockets” during the care of South Florida’s most difficult and complex cases. Recognizing the financial burden on the University from this arrangement, the State of Florida granted SI in November 2011 to the more than 900 University of Miami medical school faculty physicians who practice at the 1,600 bed JMH. The same 900 clinically active employed physicians were on staff at the University’s privately-owned, 560 bed, University of Miami Hospital (UMH) and continued to practice there without SI.
References
- Pronovost PJ. Toward eliminating all harms. Quality Management in Health Care. 2016;25(3):185-186.
- Makary MA, Daniel M. Medical error – the third leading cause of death in the US. British Medical Journal. 2016;353:i2139.
- Reed TL, Levy D, Steen LT, Roach J, Taylor T, Call K, et al. Adverse event triggered event reporting for devices. Journal of Clinical Engineering. 2016;41(2):83-89.
- Hicks CW, Rosen M, Hobson DB, Ko C, Wick EC. Improving safety and quality of care with enhanced teamwork through operating room briefings. The Journal of the American Medical Association: Surgery. 2014;149(8):863-868.
- Birnbach DJ, Rosen LF, Williams L, Fitzpatrick M, Lubarsky DA, Menna JD. A framework for patient safety: a defense nuclear industry-based high-reliability model. Joint Commission on Journal on Quality and Patient Safety. 2013;39(5):233-240.
- Middleton B, Bloomrosen M, Dente MA, Hashmat B, Koppel R, Overhage JM, et al. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. Journal of American Medical Inform Association. 2013;20:e2-e8.
- Otieno GO, Hinako T, Motohiro A, Daisuke K, Keiko N. Measuring effectiveness of electronic medical records systems: towards building a composite index for benchmarking hospitals. International Journal of Medical Informatics. 2008;77(10):657-669.
- Porter AJ, Narimasu JY, Mulroy MF, Koehler RP. Sustainable, effective implementation of surgical preprocedural checklist: an “attestation” format for all operating team members. Jointt Commission Journal on Quality and Patient Safety. 2014;40(1):3-9.
- Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat A-HS, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. New England Journal of Medicine. 2009;360(5):491-499.
- Haynes AB, Berry WR, Gawande AA. What do we know about the safe surgery checklist now? Annals of Surgery. 2015;261(5):829-830.
- Mathews SC, Demski R, Pronovost PJ. Redefining accountability in quality and safety at academic medical centers. Quality Management in Health Care. 2016;25(4):244-247.
- Suk M. Sovereign immunity: principles and applications in medical malpractice. Clinical Orthopaedics and Related Research. 2012;470(5):1365-1369.
- Frakes M. Defensive medicine and obstetric practices. Journal of Empirical Legal Studies. 2012;(9):457-481.
- Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. New England Journal of Medicine. 2003;348(23):2281-2284.
- Baicker K, Fisher ES, Chandra A. Malpractice liability costs and the practice of medicine in the Medicare program. Health Affairs (Millwood). 2007;26(3):841-852.
- Black BS, Wagner AR, Zabinski Z. The association between patient safety indicators and medical malpractice risk: evidence from Florida and Texas. American Journal of Health Economics. 2017;3(2):109-139.
- Sklar DP. Changing the medical malpractice system to align with what we know about patient safety and quality improvement. Academic Medicine. 2017;92(7):891-894.
- Mello MM, Kachalia A. Medical malpractice: evidence on reform alternatives and claims involving elderly patients. Medicare Payment Advisory Commission. http://www.medpac.gov/docs/default-source/reports/dec16_medicalmalpractice_medpac_contractor.pdf. Published December 2016.
- Dhankhar P, Khan MM, Bagga S. Effect of medical malpractice on resource use and mortality of AMI patients. Journal of Empirical Legal Studies. 2007;4(1):163-183.
- Shurtz I. The impact of medical errors on physician behavior: evidence from malpractice litigation. Journal of Health Economics. 2013;32:331-340.
- Stewart RM, Geoghegan K, Myers JG, Sirinek KR, Corneille MG, Mueller D, et al. Malpractice risk and cost are significantly reduced after tort reform. Journal of the American College of Surgeons. 201;212(4):463-469. e1-e42.
- McGwin G Jr, Wilson SL, Bailes J, Pritchett P, Rue LW 3rd. Malpractice risk: trauma care versus other surgical and medical specialties. The Journal of Trauma: Injury, Infection, and Critical Care. 2008;64(3):607-613.
- Encinosa WE, Hellinger FJ. Have state caps on malpractice awards increased the supply of physicians? Health Affairs. 2005;24:W5-250-W5-258.
- Thomas JW, Ziller EC, Thayer DA. Low costs of defensive medicine, small savings from tort reform. Health Aff (Millwood). 2010;29(9):1578-1584.
- Illingworth KD, Shaha SH, Tzeng TH, Sinha MS, Saleh KJ. The impact of tort reform and quality improvements on medical liability claims: a tale of two states. American Journal of Medical Quality. 2015;30(3):263-270.
- Avraham R, Schanzenbach M. The impact of tort reform on intensity of treatment: evidence from heart patients. Journal of Health Economics. 2015;39:273-288.
- Kessler DP, McClellan MB. How liability law affects medical productivity. Journal of Health Economics. 2002;21:931-955.
- Baicker K, Chandra A. The effect of malpractice liability on the delivery of health care. Forum for Health Economics and Policy. 2005;8(1). https://doi.org/10.2202/1558-9544.1010.
- Currie J, MacLeod WB. First do no harm? Tort reform and birth outcomes. The Quarterly Journal of Economics. 2008;132(1):795-830.
- Wu AW, Steckelberg RC. Medical error, incident investigation and the second victim: doing better but feeling worse? BMJ Quality and Safety. 2012;21(4):267-270.
- Kachalia A, Mello MM. New directions in medical liability reform. New England Journal of Medicine. 2011;364(16):1564-1572.
Table 1. Log linear model estimates
| Estimate | RR | p-value | ||
| Hospital | JMH | 0.2946 | 1.3426 | <0.0001 |
| UMH | – | – | – | |
| Post SI | ||||
| Years | Post | -0.1368 | 0.8721 | 0.0109 |
| Pre | – | – | – | |
| Individual post-years | ||||
| Years | 2012 | 0.0059 | 1.0059 | 0.9373 |
| 2013 | -0.1851 | 0.8310 | 0.0195 | |
| 2014 | 0.0658 | 1.0680 | 0.3688 | |
| 2015 | -0.4339 | 0.6480 | <0.0001 | |
| Pre | – | – | – | |
| Legend: RR = Rate ratio. A negative estimate with a significant p value means there was a significantly lower rate of serious harm events. |
Table 2
|
Case Mix Index |
||
| Year | University of Miami Hospital | Jackson Memorial Hospital |
| 2010 | 1.5533 | 1.364 |
| 2011 | 1.5651 | 1.392 |
| 2012 | 1.5824 | 1.401 |
| 2013 | 1.5841 | 1.434 |
| 2014 | 1.5872 | 1.443 |
| 2015 | 1.6054 | 1.523 |
Figure 1: Purpose of the Public Health Trust
The purpose(s) of the Trust shall include operation, governance, and maintenance of Trust facilities:
For the benefit of the general community and not for the exclusive benefit of any single individual or group of individuals; As the major provider of health services, directly and indirectly, to the poor and near poor with-in Miami-Dade County; For serving the health care needs of patients living in reasonable geographic proximity to Jackson Memorial Hospital and other Trust Facilities; With the capability of supporting, maintaining and managing a proper balance between primary, secondary and tertiary health care programs that will strive for a single standard of general and specialized health services; As a major referral center which has elected to offer a full range of medical and support specialties which are not generally available at community hospitals, including trauma care; As a teaching facility which operates training programs for physicians, nurses and other health care professionals; For providing major clinical facilities which support the University of Miami School of Medicine and other educational institutions, which train future health care professionals; and For providing opportunities for clinical and applied research in all areas of medicine to continuously upgrade the general level of medical care available to citizens. The purpose(s) of the Trust shall also include:
Participation in activities designed to promote the general health of the community; Providing recommendations to the Commission for the establishment of health care delivery policies in the designated facilities of the Trust; and Fulfillment of the objectives set forth by the Commission in the Trust Ordinance and compliance with County-wide health care delivery policies which have been or may be established by the Commission.
The purpose(s) of the Trust shall include operation, governance, and maintenance of Trust facilities:
For the benefit of the general community and not for the exclusive benefit of any single individual or group of individuals;
As the major provider of health services, directly and indirectly, to the poor and near poor with-in Miami-Dade County;
For serving the health care needs of patients living in reasonable geographic proximity to Jackson Memorial Hospital and other Trust Facilities;
With the capability of supporting, maintaining and managing a proper balance between primary, secondary and tertiary health care programs that will strive for a single standard of general and specialized health services;
As a major referral center which has elected to offer a full range of medical and support specialties which are not generally available at community hospitals, including trauma care;
As a teaching facility which operates training programs for physicians, nurses and other health care professionals;
For providing major clinical facilities which support the University of Miami School of Medicine and other educational institutions, which train future health care professionals; and
For providing opportunities for clinical and applied research in all areas of medicine to continuously upgrade the general level of medical care available to citizens.
Figure 2 A
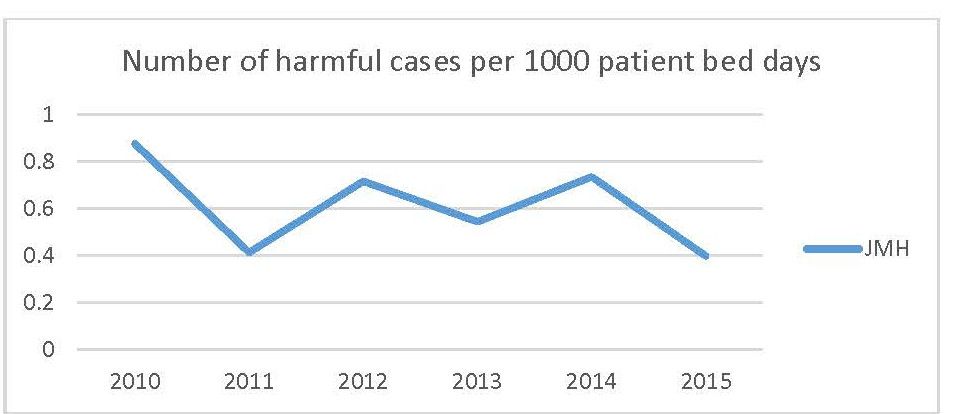
Figure 2 B
 Legend: Rate per 1000 patient bed days of Quantros G, H, and I reports per 1000 patient bed days by year.
Legend: Rate per 1000 patient bed days of Quantros G, H, and I reports per 1000 patient bed days by year.
Appendix: Statistical Analysis
Quantros report summaries with graded harm were available from 2010 to 2015 at both JMH and UMH. Serious harm was defined as category G, H, and I in the Quantros system (Table 1). In order to assess the effect of SI, the incidence of serious harm reports/patient bed day (Figure 2A) was used as an outcome in a log linear model using the log of patient bed days as the offset to account for unequal exposure to potential harm in each year. A binary time, pre-post SI, and a hospital indication (JMH or UMH) were included as independent variables.
The pre-sovereign immunity period in the pre-post SI variable was defined as pre-years (2010 and 2011), and the post-years, combining incidence of harm for 2012-2015. This two category grouping was chosen a priori to specifically compare incidence before and after the point of SI implementation. Pre vs post sovereign immunity incidence rates were evaluated, controlling for hospital trends over time by using an interaction term for JMH vs. UMH.
The interaction term was first examined between hospital and year while keeping both variables binary to evaluate whether SI’s effect on the incidence of harmful reports differed between hospitals. The interaction term was not significant (χ2=1.28; p=0.2580) and was dropped from the final model. A contrast was also conducted for the pre-sovereign immunity period vs each year of the post SI period a posteriori as well to see how individual post year was compared to the pre-years to make sure early or late temporal trends in behavior were not masked by the overall result. Contrast weights were evenly-distributed among each post SI year.
Our approach involves fitting a log-linear model to estimate and test the interaction effect between pre-post SI and hospital. This allows us to estimate potentially differential effects of SI on the different hospitals, as well as test for significance in the difference between the effect of SI in the different hospitals. By incorporating the interaction term we are able to conduct the difference-in-difference estimation and testing. The model used is as followed:
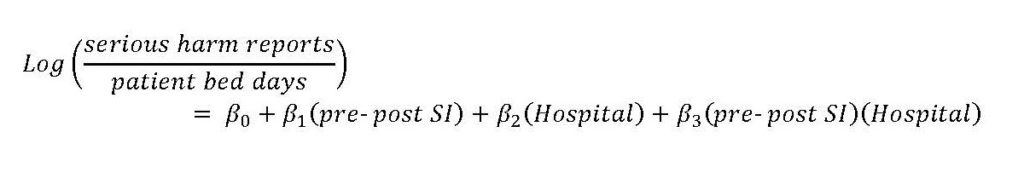
In our model, the interaction term failed to reach statistical significance, indicating that we do not have evidence to support differential effects of SI among the hospitals. For this reason, it is removed from the model and the final model used to generate the results in Table 1 is as followed:

In addition to the final model, which describes the effect of SI comparing pre vs post years as a binary variable, we also compared each individual post year to the pre years through contrast. The weights used for the contrast is as followed: pre-years (-1), 2012 (0.25), 2013 (0.25), 2014 (0.25), 2015 (0.25).
