Kelly McFarlane, BS1,2+, Teng Zhang, BA3+, Jacqueline Vallon, BS BA3+, Linying Yang, BS4, Jin Xie, BS4, Peter Glynn, PhD3, and David Scheinker, PhD3,7-9
1Stanford Graduate School of Business, Stanford, CA
2Harvard Medical School, Boston, MA
3Department of Management Science and Engineering, Stanford University School of Engineering, Stanford, CA
4Institute for Computational & Mathematical Engineering, Stanford University School of Engineering, Stanford, CA
7Clinical Excellence Research Center, Stanford University School of Medicine, Stanford, CA
8Department of Pediatrics, Stanford University School of Medicine, Stanford, CA
9Department of Perioperative Services, Lucile Packard Children’s Hospital, Stanford, CA
+These authors served as co-first authors
Contact: David Scheinker: dscheink@stanford.edu
What is the message?
Development of an interactive online tool to predict COVID-19 related demand for intensive care and acute care hospital beds can help hospitals with capacity planning.
What is the evidence?
Inputs to the online model are based on best available evidence and discussions with experts; all inputs and parameters are editable and can be updated as new data becomes available.
Link to Tool: https://surf.stanford.edu/covid-19-tools/covid-19-hospital-projections/
Timeline: Submitted April 6, 2020; accepted after revisions, April 6, 2020
Cite as: Kelly McFarlane, Teng Zhang, Jacqueline Vallon, Linying Yang, Jin Xie, Peter Glynn, and David Scheinker, 2020. Interactive Model to Estimate Bed Demand for COVID-19-Related Hospitalization Developed by Stanford Medicine-Engineering Partnership. Health Management, Policy and Innovation (HMPI.org), volume 5, Issue 1, special issue on COVID-19, April 2020.
Hospitals Dealing with COVID-19 Need to Estimate Demand for Beds and Ventilators
Hospital leaders need tools to help them prepare for a surge in COVID-19 patients in the face of limited testing capabilities as well as significant uncertainty about the rate at which COVID-19 is spreading. Intensive (ICU) and acute care (AC) beds as well as ventilators are critical for the care of COVID-19 patients. There have been severe shortages in hard-hit areas such as China, Italy, and New York.1,2 As states and hospitals scramble to open IC beds by canceling elective surgeries and purchasing more ventilators, they need to know how many beds and ventilators they will need, and when, in the coming days and weeks.
Hospital Bed Demand Projections for Capacity Planning
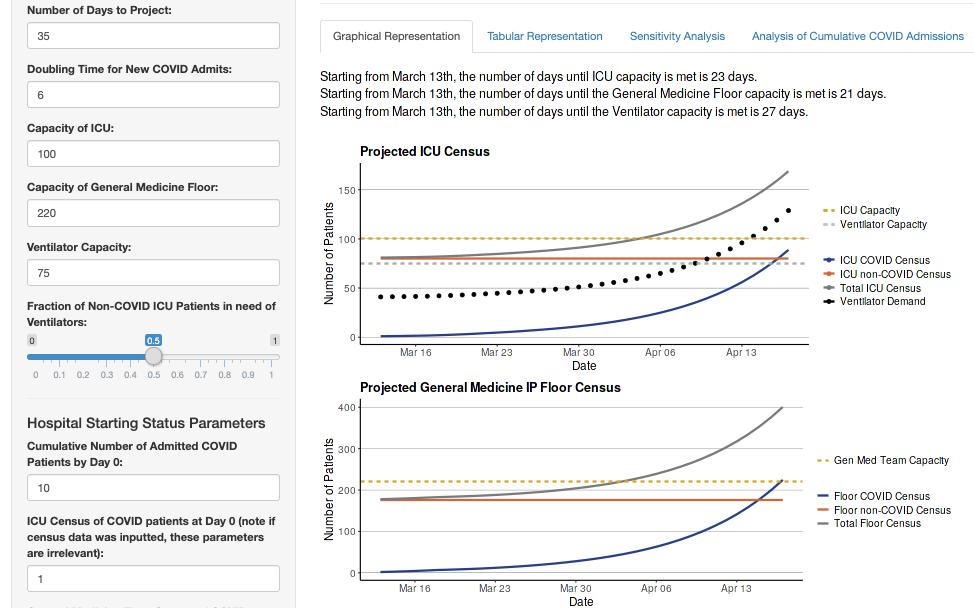
To facilitate hospital capacity planning in the presence of this uncertainty, we built an accessible, interactive model to estimate the number of IC beds, AC beds, and ventilators necessary to accommodate COVID-19 patients who require hospitalization along with the non-COVID-19 patients in the hospital.3 This model has been published as an online tool which allows users to modify the basic input parameters in order to tailor the projections to their institution.4
Hospitals leaders can input data specific to their facilities, along with estimates of the characteristics of the patient population in their region. Inputs include the starting census of COVID-19 positive and negative patients at the hospital. The estimated doubling time for total COVID-19 admissions (i.e., how many days it will take for the number of total admissions at the institution to double) is an important input to which the model is sensitive. Estimates regarding the patient length of stay and trajectory through the hospital are also inputs generated through review of existing data and discussion with experts. These parameters help to calculate how many COVID-19 patients will be in the hospital at a given time and for how long.5,6
In order to compare the projected demand to a hospital’s available resources, users can also input current capacity data including the number of IC beds, AC beds, and ventilators in the hospital in order to predict when capacity will be reached. Adjusting these capacity numbers allows the hospital to visualize the effect of different capacity expansion plans with regards to when capacity will be reached and exceeded.
An additional capability of the model is the ability to upload multiple days’ worth of census data. The model will display the current data in addition to the projections starting from the most recent date forward. This allows hospital managers to make constant adjustments to their forward projections based on what they are seeing in-house at any given time.
Value of the Model
The model is based on transparent logic and starts with simple, known inputs in addition to certain informed estimates in order to provide a robust basis of projections for hospital managers. The projections complement the many different forecast models being created for COVID-19 to help with various aspects of the uncertainties we are facing. For example, our colleagues have developed a model to calculate regional demand based on county-level hospitalization data.7 Our model similarly functions much like a calculator, helping hospitals determine their need for beds in the coming days and weeks with a manageable number of parameters and clear logic.8
The model highlights two aspects of the pandemic, concerning the rate of increase in cases and unbalanced demand for AC and IC beds. First, the estimates are particularly sensitive to the doubling time of new COVID-19 cases, emphasizing the importance of the doubling time in relation to the hospital’s ability to manage capacity; this supports the public health interventions focused on social distancing. Second, the model shows that AC beds may reach capacity before IC in certain scenarios. This is actionable information for managers who must develop and implement strategies to decrease occupancy in various parts of the hospital, such as cancelling elective procedures and accelerating efforts to cohort patients and discharge patients to appropriate step-down care facilities.
Hospitals need to address critical questions about staffing patterns and equipment capacity. This model can assist with decision-making in real-time as the epidemic unfolds.
Acknowledgements
We thank Systems Utilization Research for Stanford Medicine (https://surf.stanford.edu/) and the Clinical Excellence Research Center (http://med.stanford.edu/cerc.html) for their invaluable contributions.
Figure 1: Screen capture of tool (https://surf.stanford.edu/covid-19-tools/covid-19-hospital-projections/, accessed 04/03/2020) with permission of authors. The plot is a hypothetical situation and not a forecast for any specific hospital.
Figure 2: Screen capture of tool showing inputs for starting census, patient cohorts, and length of stay estimates (https://surf.stanford.edu/covid-19-tools/covid-19-hospital-projections/, accessed 04/03/2020) with permission of authors.
References
- Wu Z, McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. Published online February 24, 2020. doi:10.1001/jama.2020.2648
- Grasselli G, Pesenti A, Cecconi M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA. Published online March 13, 2020. doi:10.1001/jama.2020.4031
- Zhang T, McFarlane K, Vallon J, Yang L, Xie J, Blanchet J, Glynn P, Staudenmayer K, Schulman K, Scheinker D. A model to estimate bed demand for COVID-19 related hospitalization. medRxiv. https://doi.org/10.1101/2020.03.24.20042762
- SURF Stanford Medicine, Stanford University. COVID-19 Hospital ICU and Floor Census Model. https://surf.stanford.edu/covid-19-tools/covid-19-hospital-projections/ (Accessed April 2, 2020)
- Zhou, Fei, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. Published online March 11, 2020. doi:https://doi.org/10.1016/S0140-6736(20)30566-3
- Guan, Wei-jie, et al. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. Published online February 28, 2020. doi:10.1056/NEJMoa2002032
- SURF Stanford Medicine, Stanford University. Projecting Severe Cases of COVID-19. https://surf.stanford.edu/covid-19/, last accessed April 3, 2020.
- Shah, N. A calculator and a Model race to save a COVID-19 patient. Medium.com. https://medium.com/@nigam/a-calculator-and-a-model-race-to-save-a-covid19-patient-b26a40e43302, last accessed April 3, 2020.