Yeganeh Alimohammadi, Kirankumar Shiragur, Ramesh Johari, David Scheinker, Kevin Schulman, and Kristan Staudenmayer, Stanford University
Contact: kristans@stanford.edu
What is the message? The debate around school closures has focused on the question of whether schools are safe in the midst of the pandemic. Most studies look at this issue from the perspective of absolute risk. We consider the perspective of relative risk: in other words, whether children are safer at school or at home. Our model shows, under a reasonable and robust set of assumptions about testing strategies and compliance with CDC guidance on countermeasures, in-person learning can be safer for children than being at home. Interestingly, the model suggests that this benefit increases with rates of community spread. Our model-based findings are in concordance with a broad range of empirical studies suggesting that students are safe at school.
What is the evidence? Literature review and decision model.
Timeline: Submitted: February 19, 2021; accepted after revisions: February 24, 2021
Cite as: Yeganeh Alimohammadi, Kirankumar Shiragur, Ramesh Johari, David Scheinker, Kevin Schulman, and Kristan Staudenmayer. 2021. Relative-Risk and the Assessment of School Safety in the COVID-19 Pandemic: Schools May Offer Students Shelter from the Storm. Health Management, Policy, and Innovation (HMPI.org), volume 5, Issue 1, special issue on COVID-19, 2021.
School Safety: Absolute Vs. Relative Risk
The COVID pandemic has disrupted the lives and education of the children all over the world. Returning children to in-person school has become a national priority under President Biden. The opening of K-12 schools is essential for developing the next generation of our country, especially the most vulnerable.[i] The Director of the CDC has recently issued statements on the safety of school reopening.[ii] Schools have safely re-started in-person learning in many regions in the United States and in countries across the world, providing strong empirical evidence that it is possible to do so safely [iii] [iv] [v] [vi] [vii] [viii]. Yet, there remains a lingering health concern about school safety among some members of the public and some school teachers and staff.[ix]
Making sense of the health concern depend on the type of risk that one considers. The most common approaches to looking at the question of school safety focus on absolute risk. By contrast, we take the perspective that the situation warrants an approach that evaluates school safety from the perspective of relative risk: i.e., are open schools more or less safe than the surrounding community?
In looking at the problem from the perspective of relative risk, we have found a fascinating result. Under most scenarios, students would be as safe or safer in school as in their community. This is particularly true in the highest-risk communities, where many students live in households were families lack the ability to ensure socially distancing, compared to a school environment that can enforce CDC public health protocols.
Even more importantly, taking a relative risk perspective suggests that the higher the prevalence in the community, the greater the advantage offered by schools in which appropriate prevention measures are taken. This is different from much current guidance that suggests that in-person learning should stop in communities hardest hit by the pandemic. The advantage is enhanced through self-selection in which the students with the resources to remain safely at home would be more likely to do so, while those without the resources would be more likely to attend and benefit as a result.
Modeling School Safety
In this paper, we report the results of a modeling exercise to address the issue of school safety, considering three major parameters of the pandemic: community incidence, inbound infection rate, and in-school spread. Community incidence is a measure of the burden of the infection in the community. Inbound infection rate is the rate at which students infected in the community would be presenting to schools. In-school spread represents on-campus transmission of the virus. The values for these variables represent estimates that can be influenced by test accessibility, local testing culture, and vulnerability of children to become infected compared with adults[x].
“Offense” strategy: Limiting infections from entering schools
In an “offense” strategy, schools can make efforts to decrease the chance that infected students and staff come to the physical campus. Here, symptom surveys and fever checks can be deployed. However, data suggest that a large number of people remain asymptomatic after becoming infected, and even people who become symptomatic can spread the virus before symptoms appear, and might be most contagious before the onset of symptoms; symptom surveys and fever checks are inadequate to detect these infected individuals. To address this issue, testing can be deployed to identify students with asymptomatic infections. We report results based on three different testing strategies: every 3 days, every 7 days, and every 14 days.
“Defense” strategy: Mitigating risk within schools
Unfortunately, there is no foolproof testing strategy to guarantee that no infected student or staff member comes into the school environment.[xi] So, even with a testing strategy, schools need to implement a “defense” strategy applying “countermeasures.”
A defense strategy should include five mitigation approaches recommended by the CDC: (1) Universal and correct use of masks; (2) physical distancing; (3) handwashing and respiratory etiquette; (4) cleaning and maintaining healthy facilities; and (5) contact tracing in combination with isolation and quarantine.[xii] Beyond these five tactics, defense could also include assigning students to pods to limit the spread of infections, as well as environmental protections such as improved ventilation systems and ultraviolet radiation (UV-C) systems. In our model, we assess three different levels of compliance with these countermeasure bundles: low, medium and high.
Model results
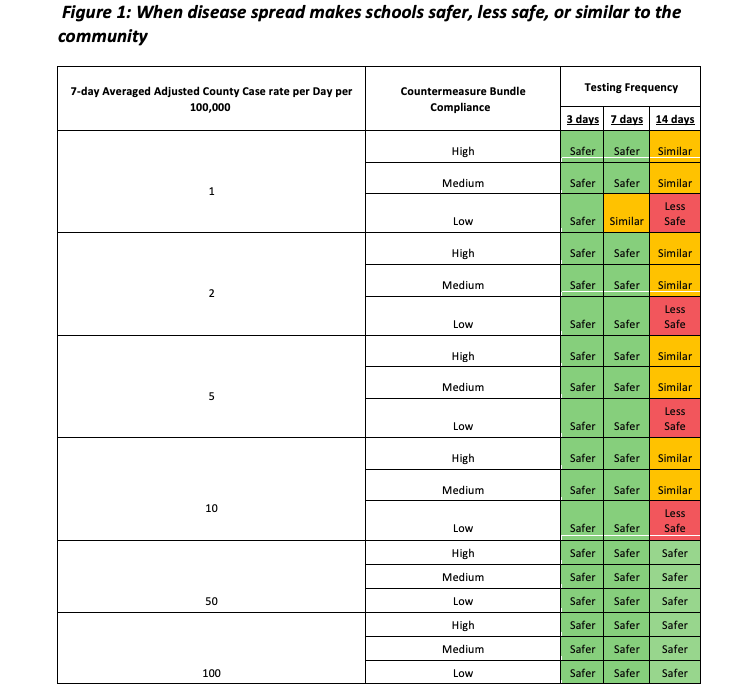
In Figure 1, we present the results of our analysis for different levels of community spread. In terms of relative risk, a school was considered to be “safer” when students would be less likely to be infected if they attend school than if they remain in the community, and was considered “less safe” if they were more likely to be infected in school than at home.
Applying this definition, when a three-day testing strategy was employed, schools were safer than the community for all levels of countermeasure bundle compliance, and for all values of the average adjusted case rate per day between 1 to 100 per 100,000. When a seven-day testing strategy was employed, the same result held, with only one exception: with an average adjusted case rate per day of 1 per 100,000 and low countermeasure bundle compliance, school and home risk would be similar.
We also considered less frequent (14 day) testing strategies. In these models, there were more scenarios where school and home would be similar risk.
We found a few scenarios in which schools were less safe than home. These primarily involved the combination of three factors”: 14-day testing, low countermeasure compliance efforts, and an average adjusted case rate per day in the community less than 10 per 100,000.
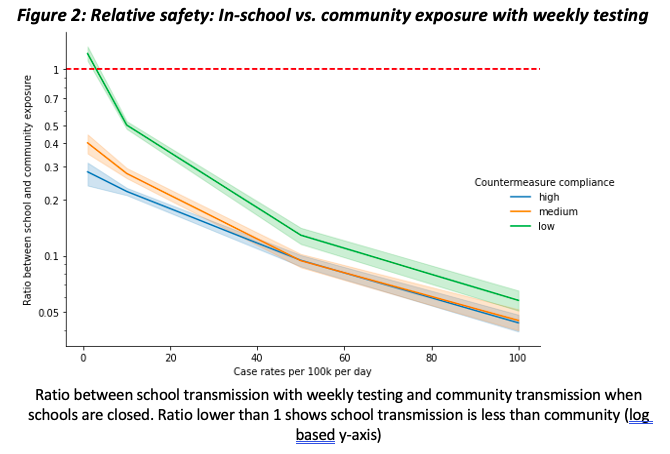
Further analysis reveal that these results are robust to a variety of assumptions. In Figure 2, we report the results of whether students are safer at home or in school with weekly testing across three different rates of school transmission.
There is a strong and intuitive implication here. When very high rates of community burden increased the community risk, schools were safer under all testing scenarios and across all compliance rates for countermeasures.
Looking Forward
The dialogue around school closures have been focused on asking the question of whether schools are safe. Our analyses strongly suggest we instead look at the issue not from an absolute risk but from a relative risk perspective. In other words, we should ask the question of whether our children are safer at school or at home. Our model is relatively robust that under a reasonable set of assumptions about testing strategies and compliance with CDC safety measures, in-person school is safer for children than being at home. Interestingly, the model suggests that this benefit increases with rates of community spread, especially for the most vulnerable children. Our model-based findings are in concordance with a broad range of empirical studies suggesting that students are safe at school.
We note two concerns that might arise in applying this relative risk framework. First is the possibility that students may spread infection into the community, having acquired it at school; this is referred to as “outbound spread” from schools. However, as the rate of school-acquired spread among students is low in nearly all scenarios with adequate testing, and testing itself detects infection among students, with resulting isolation and quarantine, the rate of outbound spread from schools would also remain low even in communities with high inbound rates.
Second, there may be some households, e.g., with particularly vulnerable individuals at home, that may wish to mitigate absolute risk by keeping kids at home. As long as schools continue to accommodate such needs, such as by continuing to offer a distance learning option, the self-selection of who does and does not attend in-person will increase the benefits of reopening schools.
This model reinforces an emerging understanding of the risks and benefits of school opening. Independently of the particular model used in this work, the results of our analysis accord with numerous reports of reported empirical data from schools that have reopened, various simulation models of school reopening, and studies finding that communities with the lowest prevalence of the virus are those in which the rates of masking, social distancing, and testing approach the levels we modeled. [xiii] [xiv] These analyses should provide reassurance to parents and teachers that our children are safer at school than at home at this point in the pandemic, but also suggest the need for careful attention to CDC guidance on countermeasures to achieve this result.
References:
[i] https://joebiden.com/reopening/
[ii] https://www.cnbc.com/2021/02/03/cdc-director-says-schools-can-safely-reopen-without-vaccinating-teachers.html; https://www.nytimes.com/2021/01/26/world/cdc-schools-reopening.html
[iii] Incidence and Secondary Transmission of SARS-CoV-2 Infections in Schools
Kanecia O. Zimmerman, Ibukunoluwa C. Akinboyo, M. Alan Brookhart, Angelique E. Boutzoukas, Kathleen McGann, Michael J. Smith, Gabriela Maradiaga Panayotti, Sarah C. Armstrong, Helen Bristow, Donna Parker, Sabrina Zadrozny, David J. Weber, Daniel K. Benjamin
Pediatrics Jan 2021, e2020048090; DOI: 10.1542/peds.2020-048090
[iv] Yoon Y, Kim KR, Park H, Kim S, Kim YJ. Stepwise School Opening and an Impact on the Epidemiology of COVID-19 in the Children. J Korean Med Sci. 2020 Nov 30;35(46):e414.; Otte Im Kampe E, Lehfeld AS, Buda S, Buchholz U, Haas W. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveill. 2020 Sep;25(38):2001645.
[v] Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 Cases and Transmission in 17 K–12 Schools — Wood County, Wisconsin, August 31–November 29, 2020. MMWR Morb Mortal Wkly Rep 2021;70:136–140. DOI: http://dx.doi.org/10.15585/mmwr.mm7004e3
[vi] Ludvigsson, JF. Children are unlikely to be the main drivers of the COVID‐19 pandemic – A systematic review. Acta Paediatr. 2020; 109: 1525– 1530. https://doi.org/10.1111/apa.15371
[vii] Hobbs CV, Martin LM, Kim SS, Kirmse BM, Haynie L, McGraw S, Byers P, Taylor KG, Patel MM, Flannery B; CDC COVID-19 Response Team. Factors Associated with Positive SARS-CoV-2 Test Results in Outpatient Health Facilities and Emergency Departments Among Children and Adolescents Aged <18 Years – Mississippi, September-November 2020. MMWR Morb Mortal Wkly Rep. 2020 Dec 18;69(50):1925-1929. doi: 10.15585/mmwr.mm6950e3. PMID: 33332298; PMCID: PMC7745952.
[viii] COVID-19 in children and the role of school settings in transmission – first update. Stockholm: ECDC; 2020.
[ix] https://www.vox.com/22254942/covid-19-schools-reopening-cases-cdc-opening
[x] Tönshoff B, Müller B, Elling R, et al. Prevalence of SARS-CoV-2 Infection in Children and Their Parents in Southwest Germany. JAMA Pediatr. Published online January 22, 2021.
[xi] Letizia AG, Ramos I, Obla A, Goforth C, Weir DL, Ge Y, Bamman MM, Dutta J, Ellis E, Estrella L, George MC, Gonzalez-Reiche AS, Graham WD, van de Guchte A, Gutierrez R, Jones F, Kalomoiri A, Lizewski R, Lizewski S, Marayag J, Marjanovic N, Millar EV, Nair VD, Nudelman G, Nunez E, Pike BL, Porter C, Regeimbal J, Rirak S, Santa Ana E, Sealfon RSG, Sebra R, Simons MP, Soares-Schanoski A, Sugiharto V, Termini M, Vangeti S, Williams C, Troyanskaya OG, van Bakel H, Sealfon SC. SARS-CoV-2 Transmission among Marine Recruits during Quarantine. N Engl J Med. 2020 Dec 17;383(25):2407-2416.
[xii] Centers for Disease Control and Prevention (CDC). Operational Strategy for K-12 Schools Through Phased Mitigation. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/operation-strategy.html
[xiii] Otte Im Kampe E, Lehfeld AS, Buda S, Buchholz U, Haas W. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveill. 2020 Sep;25(38):2001645. doi: 10.2807/1560-7917.ES.2020.25.38.2001645. PMID: 32975186; PMCID: PMC7533620.
[xiv] Exclusive: Kids catch and spread coronavirus half as much as adults, Iceland study confirms, https://www.nationalgeographic.com/science/article/we-now-know-how-much-children-spread-coronavirus