Liam Ferreira and Forest S. Kim, Robbins Institute of Health Policy, Baylor University
Contact: Liam_Ferreira1@baylor.edu
Abstract
What will you learn? Leaders are starting to appreciate the low-cost technologies and efficient delivery designs of developing nations. The DOCTOR model — delivery, outreach, cost, task-shifting, optimization, and revolutionary change — helps to educate professionals and promote the implementation of reverse innovation in the U.S. healthcare system in response to COVID-19 and other large-scale public health emergencies.
What is the evidence? The author draws on his experience and assessment of healthcare practice.
Timeline: Submitted: February 24, 2021; Accepted after review: November 5, 2021.
Cite as: Liam Ferreira and Forest Kim. Using Reverse Innovation to Improve Healthcare Management in Response to COVID-19. 2021. Health Management Policy and Innovation, Volume 6, Issue 2. Health Management, Policy and Innovation (HMPI.org), Volume 6, Issue 2.
With the advent of the coronavirus (COVID-19) pandemic, many analysts are trying to predict the associated costs for an overburdened U.S. healthcare system (1). With healthcare in the United States reaching approximately $4 trillion annually and compromising 18% of the gross domestic product (GDP), healthcare costs already represent a significant economic burden (2,3). If COVID-19 infects 20 percent of the American population, the U.S. will have to spend $163.4 billion to cover infection cases (1).
The U.S. spends slightly more than twice the average developed country in terms of GDP percentage (3). While the United States excels in academic research and leads all countries in research output, the overall health of American citizens rates poorly in most health outcomes compared to other developed nations (3). Key drivers behind healthcare inefficiencies are poor allocation and “waste” – substandard delivery, administrative complexity, and uncoordinated care (2).
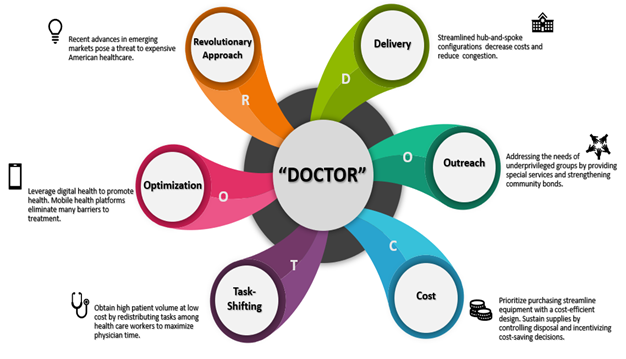
The expenditures mentioned above will escalate with the increasing demand for limited resources and supplies given the rapid rise in cases (1). Increased patient load due to a communicable disease (e.g. COVID-19) results in poor outcomes as limited physicians and healthcare professionals are available for quality patient care. Although the pandemic has encumbered the U.S. health system, COVID-19 has raised awareness for novel solutions to introduce cost-efficient delivery, provide better accessibility, and foster greater utilization of digital health (1,4). This paper educates management on healthcare needs revealed by COVID-19 that can be improved through reverse innovation via the DOCTOR model – a new framework for applying reverse innovation (please see Figures 1-2).
Figure 1
The DOCTOR Model Outlining the Implementation of Reverse Innovation in the U.S. Healthcare System
The Doctor Model
The global exchange of innovative concepts and skills has been a hallmark of civilizations throughout history (5). Different periods allowed specific regions to contribute to ideas that diffused into neighboring societies. Persia’s Ibn Sina’s expansive medical knowledge guided centuries of European science. Anti-malarials were derived from Chinese medicine. Recent history has produced conditions that enable low-income countries (LICs) to produce cost-effective solutions that subsequently diffuse to higher-income countries (HICs).
These advancements of “reverse innovation” have led many healthcare leaders to view this as a promising paradigm shift in global health (5). Constrained resources, large patient volumes, and sustainable development offer powerful incentives that fuel reverse innovation in LICs (6). Since COVID-19 has revealed many shortcomings in the U.S. healthcare systems, management can utilize elements of reverse innovation to improve the American healthcare experience.
For this paper, the author created a new framework and corresponding graphic visualization (Figure 2), the DOCTOR model, to educate professionals on applying reverse innovation in the U.S. healthcare system. “DOCTOR” is a mnemonic designed to enhance recall of the model’s main components. Each component was carefully selected based on key opportunities found in the literature where reserve innovation could be applied and result in improved outcomes.
Figure 2
Key Components of the DOCTOR Model
Delivery
Management and physicians must seek to efficiently deliver healthcare in an increasingly complex design structure. Inefficient delivery can deplete resources and lead to poor clinical outcomes (7). Hospitals in emerging markets have devised innovative design structures to maximize healthcare delivery with limited resources (8).
With a low practitioner density, high mortality rates, and per capita income of only $1,500, India would not seem like the ideal place to seek healthcare solutions (8). However, these pressing challenges have provided incentives for a few hospitals in the subcontinent to find innovative ways to deliver healthcare effectively and affordably. The most notable innovative hospital system is Narayana Health, but other hospital chains such as Deccan Hospital and Healthcare Global Enterprises Ltd. (HCG) maximize delivery via a hub-and-spoke design (8).
The hub-and-spoke configuration allows the hospital to focus on talent and resources in the main “hub” while introducing “spokes” to maximize outreach (8). Spoke facilities serve as gatekeepers, deliver diagnoses, and offer places for follow-up treatments. Rather than miniature duplicated hospitals (as seen in the U.S.), this design streamlines costs by channeling patients into the main hub for surgical procedures / treatments requiring top-talent. For example, HCG has many specialists and expensive instruments (e.g. cyclotrons, PET) concentrated in hubs at major cities (e.g. Mumbai, Bangalore) while spokes with less expensive equipment are spread out to maximize reach and generate high patient volumes. Telemedicine further extends the reach of spokes, limiting distance barriers and saving costs of unnecessary equipment, personnel, and tests incurred by the hospitals (8).
High patient volume and streamlined configuration allow these hospitals to decrease cost and increase quality (8). Doctors are constantly exposed to large volumes with considerable variety, improving diagnosing capacity and attracting talented doctors and medical students. Because of a smoothly functioning delivery system, the hospitals can standardize protocols and tailor innovation to patients’ needs in an affordable manner (8).
COVID-19 has exposed the need for a hub-and-spoke design that can streamline costs and decrease congestion (7,9). The hub-and-spoke design offers expanded market coverage and can quickly direct patients to the central hub without duplicating equipment (7). Proper screening can keep patients from seeking unnecessary care at the hub. This design is easily scalable as certain additional spokes can be added (7). With increased acceptance of telehealth during COVID-19 (10), management should utilize this opportunity to adopt the hub-and-spoke delivery design. Management should also consider funding transport systems that minimize contact to facilitate movement between hub and spokes while minimizing COVD-19 transmission.
Outreach
While delivery designs occupy an integral role in reverse innovation, outreach helps ensure that heavily burdened populations are properly treated. Before the pandemic, significant and ingrained disparities in healthcare treatment and outcomes existed in the U.S. (11). COVID-19 has intensified these disparities, drawing attention to the inequalities that continue to plague the U.S. healthcare system. Marginalized communities (e.g. Black, Hispanic, American Indian) have infection rates and mortality rates more than double the rates of Caucasians. COVID-19 forced America to seek innovative ideas to maximize outreach to these communities (11). Emerging markets offer potential solutions by leveraging opportunities to not only reach underserved populations but also forge strong bonds with communities.
East Africa has a significant rural population; however, these underserved segments are separated by harsh terrain (12). Poor roads and increased delivery costs hamper the efficient delivery of supplies. The Rwandan government responded to this pressing concern by partnering with Zipline International Inc. to develop drones dedicated to delivering supplies, such as platelets, to unreached areas. With a simple WhatsApp® message, doctors can dispatch Zips to distribute supplies within a 75 km radius (12). The Rwandan Ministry of Health has also invested in training the local personnel at these limited rural health centers to ensure quality treatment (13,14). Investing in healthcare training programs at these sites can equip local mentors with expertise and a strong affinity to underserved communities (14).
Brazil has experienced an increase in the prevalence of chronic disease and hospital burden (15). In response, the government created the Family Health Strategy to provide preventative care across the nation (16). Community Health Workers (CHWs) make routine visits to each house in their designated area for a month, to offer primary care (16). CHWs direct the patients to a local clinic and promote activities that actively engage all community members in poor communities (17). Brazil’s program has decreased ambulatory hospitalization rates and increased community awareness, especially in impoverished regions (15,17).
Aravind Eye Hospital was established by Dr. Venkataswamy to eliminate preventable blindness in South India by targeting underserved populations, the poor, and rural inhabitants (18). Although Aravind offered free treatments to these underserved populations, transportation costs for the patient hindered many from making the trip. A report revealed that only 14.6% of patients counseled to undergo surgery had the procedure. Aravind provided free food and transportation to and from the hospital. To increase outreach, Aravind also recruits patient counselors from these rural areas who provide a common link between these communities and hospitals. The counselors are selected for communication and empathy to strengthen trust and participation (18).
Truly addressing the needs of underprivileged groups extends beyond addressing “cultural competencies” (19); management must spend the effort to understand community needs and develop a strong rapport with the patient. Management must strategically invest in community mediators and patient perception to better overcome barriers to treatment. By effectively addressing these needs and equipping communities to surmount barriers, management can decrease the disease burden and improve precautionary measures to prevent the spread of communicable diseases such as COVID-19.
Cost
The pandemic continues to raise the question: how can management find innovative solutions to provide accessible and affordable care? The ventilator shortage is one of the many issues that have called for agility in acquiring devices and controlling costs (20). This section will explore how hospitals can leverage these opportunities to control cost by assessing purchase criteria, eliminating unnecessary spending, and incentivizing cost-saving decisions.
To effectively deliver care at affordable rates, innovators in emerging markets have been forced to produce innovations with cost as the limiting reagent (6). Constrained by price, innovators developed devices and treatment regimens that offer both accessibility and quality (6). For example, General Electric developed a handheld electrocardiogram (ECG), the GE Mac 400 series, to meet the constraints of rural India (21). The design team excluded superfluous features to yield a low-cost but quality ECG suitable for high patient volumes. Most importantly, the unit’s streamlined design allows it to sell at an affordable price ($1,000 vs traditional unit price of $2,000 – $10,000) (21).
The acceptance of this ECG in the U.S. has led management to reflect on prior expenditures on exorbitantly priced equipment that complete the task as efficiently as the affordable Mac 400. In the future, multiple purchase criteria should be considered by the hospital financial department (22). Instead of purchasing devices based on competing with rival hospitals, management should analyze a purchase across many different metrics, chiefly cost. Management should consider the unit cost, coverage, clinical benefit, and the cost per patient before purchasing expensive medical equipment (22). Proper technology assessment can eliminate unnecessary spending and prompt suppliers to provide cost-efficient designs, as seen with the Mac 400 series.
After re-examining purchase criteria, management must also consider eliminating unnecessary spending. Instead of discarding medical equipment, many innovative hospitals in India have carefully controlled costs while maintaining high-quality by maximizing equipment lifespan and eliminating unnecessary waste (8). Narayana Health and CARE hospitals do not discard the steel clamps ($160) utilized during cardiothoracic surgery (8) without compromising quality. Apollo Hospitals decreased suture length to control costs after noticing that surgeons do not use the allocated suture length and dispose of the remainder. Many hospital chains have even developed their own low-cost products. CARE Hospitals developed affordable cardiology equipment (8); Aravind Eye Care pioneered affordable contacts by designing Aurolab (8,18).
COVID-19 underscored the importance of controlling costs while sustaining limited medical supplies (20). The increasing demand and lack of available PPE have forced many hospitals to reevaluate their current spending. Instead of discarding equipment, hospitals are reusing equipment while maintaining sanitation (20). To prepare for a wave of a communicable disease, management can control unnecessary waste and prioritize sustainability, such as reusable textiles (23). For example, revaluating supplies in ICU carts has been shown to eliminate wasted supplies by 63% (24).
Lastly, management can lower hospital costs by incentivizing cost-saving decisions by the entire patient-care team (25). Protocols should be implemented to conserve reusable equipment and eliminate unnecessary waste. At Narayana Health, management follows this strategy by sending doctors text messages detailing expenses the day after completed procedures (8). Ultimately, management in the U.S. should implement strategies to create an awareness of the costs and incentives for cost-efficiency (8).
Task-Shifting
Physicians in the U.S. frequently claim that they have reduced patient interaction; most of their time is spent on copious amounts of paperwork instead of attending to patients (26). Many have encouraged a restructuring of tasks among other healthcare works to alleviate the burden and boost productivity (26). During COVID, the limited number of doctors relative to the large patient burden has revealed the urgent need for task-shifting (27).
Over two-thirds of HIV/AIDS cases are in Sub-Saharan Africa, yet this region only has 3% of health workers (28). With limited capital and low physician density, these countries have used task-shifting to improve clinical outcomes (29,30). Proper training of non-physician medical staff has been shown to increase antiretroviral therapy (ART) adherence and increase T cell counts (29). Just as the implementation of task-shifting yields promising outcomes for African patients, India has also reached unprecedented levels of efficiency with task-shifting.
India is significantly constrained by the scarcity of physicians relative to its large population size (31). Aravind Eye Care has responded to these constraints by implementing task-shifting to maximize the limited number of physicians (32). Aravind’s model of high-volume, assembly-line setup, and “McDonaldization of health,” has led to significant improvements in eye-care (31,32). Doctors do not have to spend crucial time on mindless paperwork or preparing the patient (32). Instead, other health workers with lower skillsets assume these roles and prepare the patient for surgery. Strict checklists to standardize hospital operations and a high-efficiency assembly line set-up allow for cataract surgery to be performed in five minutes. Aravind doctors improve clinical outcomes through high patient volumes (2,000 cataract procedures annually versus the 500 cataract procedures in the U.S.). Additionally, task-shifting allows for physicians to care for individuals who previously might not have been able to afford treatments (32).
Heralded as the Henry Ford of heart surgery, Dr. Devi Shetty, founder, and CEO of Narayana Health also champions this approach (8). By optimizing outcomes, Narayana Health improves efficiency by reducing physician time between patients and redistributing tasks to other healthcare workers. Narayana also equips patients and their families with video lectures on postoperative care before hospital discharge, to decrease unnecessary visits. The overall effect of this streamlined system is reduced expenditures, fewer complications, and treatment adherence (8).
COVID-19 has revealed the need for systems that maximize time spent with physicians. During the pandemic, other healthcare workers have been trained to perform tasks to relieve the burden (33). However, this rapid restructuring of medical tasks among healthcare workers without necessary acclimatization has consequences. Personnel report high levels of exhaustion and burnout during the restructuring process (33). How can management effectively implement task-shifting to prepare for a second wave or future pandemics? Management should standardize hospital procedures and restructure tasks to ensure that hospital personnel is performing to their maximum capacity in relevant tasks. Most importantly, management should administer training to facilitate the transition and improve overall efficiency.
Optimization
COVID-19 has underscored the importance of leveraging digital technology to promote better health (4). Ushahidi® began in Kenya as a crowdsourcing platform to record eye-witness accounts of violence following the election of 2008 (6). Ushahidi® gathered data from cell-phones, mapped the data, and deployed the information for community needs. It was later used in the 2010 Haiti earthquake and eventually diffused into the U.S.in the Deepwater Horizon crisis. Emerging markets using solutions like Ushahidi® succeed by empowering the patient (6).
While resources in developing nations remain a limiting reagent, mobile technology has achieved significant penetration within these markets (34). Healthcare leaders are using the prevalence of mobile phones to their advantage. Leaders are optimizing healthcare by providing affordable, convenient, and transparent treatment to patients via mobile health (mHealth). Babyl Rwanda™ optimizes care through digital health. Babyl™ allows customers to send SMS to request an appointment, transmit payments with mobile money, and complete follow-ups with healthcare professionals. While it does incentivize the usage of healthcare services, Babyl™ also serves to inform the community of real-time changes in certain outbreaks. Both CHWs and laypeople can use this app to update the community on a surge of disease incidents (34).
In addition to providing awareness to current health issues, mHealth also provides long-term benefits to patients (35). Patients become more actively involved in their health; they can easily reach healthcare professionals. Most importantly, mHealth increases patient adherence to routine reminders and supplementary consultation. Much of mHealth’s success can be attributed to tailoring the approach to meet local community needs. The patient develops a stronger connection to the healthcare providers; this strong association facilitates the relay of health information to the patient (35).
Management should utilize awareness for mHealth in COVID-19 to optimize existing systems. mHealth should provide convenient and accessible platforms that eliminate barriers to treatment for all patients. Instead of merely stopping at telehealth, management should provide mHealth incentives for adherence and follow-up to achieve long-term outcomes and maintain a stable supply of patients within a system. Successful mHealth patterns in emerging markets stem from strong trust within communities. Management should segment patient groups and find tangible ways to foster community relations during mHealth implementation.
Revolutionary Change
Advances in emerging markets offer cost-effective solutions to the U.S. healthcare system. Will American management start to incorporate practices of reverse innovation into the healthcare system? COVID-19 has demonstrated a pressing need for reform. The pandemic has revealed short-comings of a burdened system. COVID-19 has forced reimbursement changes in digital health (36), but the pandemic calls for radical change to healthcare.
Ultimately, finances (reimbursement) largely pave the way for healthcare changes. Reverse innovation offers a cost-effective alternative to several dimensions of expensive American healthcare. While most examples in this paper focused on emerging markets in South Asia, Africa, and South America, reverse innovation has now come to the doorsteps of America – threatening to steal significant market share from American hospitals.
In 2014, Narayana Health opened its first multispecialty hospital in the Cayman Islands (37). This strategic location with a short flight from the U.S. allows Americans to receive quality care at an affordable price (8). Accreditation by the Joint Commission further confirms Narayana’s high-quality, yet cost-effective healthcare system (38). Narayana’s Cayman hospital and the changes during the pandemic could serve as a “Blockbuster Video moment.” Just as executives at Blockbuster were too late in adapting to changes in the home entertainment industry (i.e., on-demand streaming), ultimately resulting in Blockbuster’s bankruptcy, the U.S. might face a precarious situation if management ignores advancements of reverse innovation. Management must break from a complacent approach and actively seek ways to effectively implement these emerging healthcare solutions found in developing nations.
Look Forward
The unprecedented COVID-19 pandemic has revealed the need for improvements in hospital management. Management and healthcare professionals can utilize aspects of reverse innovation to provide better healthcare for all Americans. This paper provided a new framework, the author’s DOCTOR model, to help give a comprehensive understanding of the benefits of reverse innovation.
Streamlined hub-and-spoke delivery configurations can decrease costs and reduce congestion. Management should address the needs of underserved groups by providing special services and strengthening community trust. Management should prioritize purchasing streamlined equipment and controlling costs. Proper implementation of task-shifting yields high volumes by maximizing physician time and restructuring tasks. Management must use COVID-19 to leverage mHealth platforms to eliminate barriers.
Ultimately, recent advances in emerging markets pose a threat to an unaffordable American healthcare system. While this paper mainly explored examples of reverse innovation in India, Africa, and South America, future researchers could mine successful reverse innovation opportunities in several other regions such as Southeast Asia. This region often bears the initial impact of epidemics from the coronavirus subfamily (39); a comprehensive analysis could reveal how reverse innovation helps the region combat communicable diseases.
References
- Bartsch SM, Ferguson MC, McKinnell JA, O’Shea KJ, Wedlock PT, Siegmund SS, et al. The Potential Health Care Costs And Resource Use Associated With COVID-19 In The United States. Health Affairs (Millwood). 2020;39(6):927–35.
- Garg S. The ‘“ Economic Health ”’ of U .S . Health Care. Diabetes Technology & Therapeutics. 2020;22(2):136–41.
- Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA – Journal of the American Medical Association. 2019;322(15):1501–9.
- Torous J, Myrick KJ, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: Using technology today to accelerate the curve on access and quality tomorrow. Journal of Medical Internet Research. 2020;22(3):1–6.
- Syed SB, Dadwal V, Martin G. Reverse innovation in global health systems: Towards global innovation flow. Global Health. 2013;9(1):9–10.
- DePasse JW, Lee PT. A model for “reverse innovation” in health care. Global Health. 2013;9(1).
- Elrod JK, Fortenberry JL. The hub-and-spoke organization design: An avenue for serving patients well. BMC Health Service Research. 2017;17(Suppl 1).
- Ramamurti R. Delivering World- Class Health Care , Affordably Delivering World-Class. Harvard Business Review. 2015;(August 2014).
- Fong ZV, Qadan M, Jr RM, Griggs CL, Shah PC, Buyske J, et al. Practical Implications of Novel Coronavirus COVID-19 on Hospital Operations , Board Certification , and Medical Education in Surgery in the USA. Journal Gastrointestinal Surgery. 2020;1232–6.
- Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA, Huiart L. Digital health strategies to fight COVID-19 worldwide: Challenges, recommendations, and a call for papers. Journal of Medical Internet Research. 2020;22(6).
- Michener L, Aguilar-gaxiola S, Alberti PM, Castaneda MJ, Castrucci BC, Harrison LM, et al. Engaging With Communities — Lessons (Re)Learned From COVID-19. Preventing Chronic Disease: Public Health Research, Practice, and Policy. 2020;1–8.
- Ackerman E, Strickland E. Medical delivery drones take flight in east Africa. IEEE Spectrum. 2018;55(1):34–5.
- Binagwaho A, Nutt CT, Mutabazi V, Karema C, Nsanzimana S, Gasana M, et al. Shared learning in an interconnected world : innovations to advance global health equity. Global Health. 2013;1–5.
- Anatole M, Magge H, Redditt V, Karamaga A, Niyonzima S, Drobac P, et al. Nurse mentorship to improve the quality of health care delivery in rural Rwanda. Nursing Outlook [Internet]. 2013;61(3):137–44. Available from: http://dx.doi.org/10.1016/j.outlook.2012.10.003
- Macinko J, Dourado I, Aquino R, de Fátima Bonolo P, Lima-Costa MF, Medina MG, et al. Major expansion of primary care in Brazil linked to decline in unnecessary hospitalization. Health Affairs. 2010;29(12):2149–60.
- Johnson CD, Noyes J, Haines A, Thomas K, Stockport C, Ribas AN, et al. Learning from the Brazilian community health worker model in North Wales. Global Health. 2013;9:25.
- Rocha R, Soares RR. EVALUATING THE IMPACT OF COMMUNITY-BASED HEALTH INTERVENTIONS : EVIDENCE FROM BRAZIL’S FAMILY HEALTH PROGRAM. Health Economics. 2010;158(May):126–58.
- Ravilla T. The Story of Innovation at Aravind Eye Care System [Internet]. LDA Journal of Management. 2014. p. 26–36. Available from: https://aravind.org/wp-content/uploads/2019/04/The-Story-of-Innovation-at-Aravind-Eye-Care-System.pdf
- Kleinman A, Benson P. Anthropology in the clinic: The problem of cultural competency and how to fix it. PLoS Med. 2006;3(10):1673–6.
- Mirchandani P. Health Care Supply Chains: COVID-19 Challenges and Pressing Actions. Annals of Internal Medicine. 2020;173(4):300–1.
- Skopec M, Issa H, Harris M. Delivering cost effective healthcare through reverse innovation. BMJ. 2019;367(November):1–5.
- Martelli N, Hansen P, van den Brink H, Boudard A, Cordonnier AL, Devaux C, et al. Combining multi-criteria decision analysis and mini-health technology assessment: A funding decision-support tool for medical devices in a university hospital setting. Journal Biomedical Informatics [Internet]. 2016;59:201–8. Available from: http://dx.doi.org/10.1016/j.jbi.2015.12.002
- Overcash M. A comparison of reusable and disposable perioperative textiles: Sustainability state-of-the-art 2012. Anesthesia Analgesia. 2012;114(5):1055–66.
- Cockerham M, Haverland A, Solvang N, Cullen L. Battling Supply Waste in the ICU: A Bedside Cart Standardization Project. Journal of Perianesthesia Nursing [Internet]. 2016;31(1):89–94. Available from: http://dx.doi.org/10.1016/j.jopan.2015.11.003
- Eiferman D, Bhakta A, Khan S. Implementation of a shared-savings program for surgical supplies decreases inventory cost. Surgery (United States) [Internet]. 2015;158(4):996–1002. Available from: http://dx.doi.org/10.1016/j.surg.2015.06.010
- Ahmed F, Ahmed N, Briggs TWR, Pronovost PJ, Shetty DP, Jha AK, et al. Can reverse innovation catalyse better value health care? Lancet Global Health [Internet]. 2017;5(10):e967–8. Available from: http://dx.doi.org/10.1016/S2214-109X(17)30324-8
- Mobula LM, Heller DJ, Commodore-Mensah Y, Walker Harris V, Cooper LA. Protecting the vulnerable during COVID-19: Treating and preventing chronic disease disparities. Gates Open Research. 2020;4:125.
- Selke HM, Kimaiyo S, Sidle JE, Vedanthan R, Tierney WM, Shen C, et al. Task-shifting of antiretroviral delivery from health care workers to persons living with HIV/AIDS: Clinical outcomes of a community-based program in Kenya. Journal of Acquired Immune Deficiency Syndromes. 2010;55(4):483–90.
- Shumbusho F, Griensven J Van, Lowrance D, Turate I, Weaver MA, Price J, et al. Task Shifting for Scale-up of HIV Care : Evaluation of Nurse-Centered Antiretroviral Treatment at Rural Health Centers in Rwanda. PLoS Medicine. 2009;6(10):1–12.
- Callaghan M, Ford N, Schneider H. A systematic review of task- shifting for HIV treatment and care in Africa. Human Resources for Health. 2010;8.
- Rangan VK. The Aravind Eye Hospital , Madurai , India : In Service for Sight. World Health. 2009;215–34.
- Nandini AS, Guruprasad L. Aravind Eye Care systems : A Model with a Vision of gifting eye sight to the Aravind Eye Care systems : A Model with a Vision of gifting eye sight to the Needy. BMS College of Engineering. 2014;(October).
- Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. Articles The experiences of health-care providers during the COVID-19 crisis in China : a qualitative study. Lancet Global Health [Internet]. 2020;8(6):e790–8. Available from: http://dx.doi.org/10.1016/S2214-109X(20)30204-7
- Uwaliraye P, Ndimubanzi P, Muhire A, Lyle V. Integration of Health and Medical Innovations in Rwanda To Promote Health Equity. Global Innovation Index 2019. 2019;177–82.
- Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health. 2014;14(1).
- Keesara S, Jonas A, Schulman K. Covid-19 and Health Care’s Digital Revolution. New England Journal of Medicine. 2020;82(1):22–4.
- Gupta B, Khanna T. A recombination-based internationalization model: Evidence from Narayana Health’s journey from India to the Cayman Islands. Organization Science. 2019;30(2):405–25.
- Govindarajan V, Ramamurti R. Is This the Hospital That Will Finally Push the Expensive U.S. Healthcare System to Innovate? Harvard Business Review. 2018;
- Lim JT, Dickens BSL, Choo ELW, Chew LZX, Koo JRH, Tam C, et al. Revealing regional disparities in the transmission potential of SARS-CoV-2 from interventions in Southeast Asia: SARS-CoV-2 regional disparities. Proceedings of the Royal Society B: Biological Sciences. 2020;287(1933).