Devin A. Stone, Jennifer A. Ohn, Luis Arzaluz, and Mara B. McDermott, McDermott+Consulting
Contact: DAStone@mcdermottplus.com
Abstract
What is the message? During the pandemic, telehealth provided Medicare patients access to care and helped minimize their exposure to COVID-19. Post pandemic, telehealth has the potential to provide a promising pathway to achieve improved and equitable access to care, and to help mitigate the current healthcare workforce shortage. Congress should therefore consider proposals to extend telehealth flexibilities beyond the pandemic public health emergency.
What is the evidence? U.S. government Medicare administrative claims data documenting telehealth utilization among Medicare fee-for-service beneficiaries, as well as American Community Survey data from the U.S. Census on broadband access in counties nationwide.
Timeline: Submitted: July 18, 2022; accepted after review: October 1, 2022.
Cite as: Devin A. Stone, Jennifer A. Ohn, Luis Arzaluz, Mara B. McDermott. 2022.Telehealth’s Role In Preserving Access for Medicare Beneficiaries During the Public Health Emergency. Health Management, Policy and Innovation (www.HMPI.org), Volume 7, Issue 3.
Introduction
Spurred by the COVID-19 pandemic during which patients needed to find care that was safe and effective, while also helping to “flatten the curve,”[1] telehealth provided an important avenue for patients to maintain access to care and for both patients and providers to avoid unnecessary exposure to the virus.[2] Out of necessity, telehealth was adopted at a rapid clip, with over 14 million Medicare fee-for-service (FFS) beneficiaries receiving care via telehealth in 2020, compared to fewer than 211,000 Medicare FFS beneficiaries in the year prior. Telehealth was commonly used by patients regardless of their age, sex, race, and ethnicity, but upon closer analysis, telehealth was most commonly used by patient groups that traditionally incur high healthcare costs.[3] Through the rapid proliferation of telehealth services, this mode of care delivery has proven to not only maintain care access and mitigate the spread of infection by minimizing COVID-19 exposure, but it has delivered cost-effective and efficient care.[2] Furthermore, telehealth presents the potential to improve overall access to healthcare services. [2],[4] In this paper, we analyze the impact of the COVID-19 pandemic on telehealth utilization among Medicare beneficiaries and the telehealth policy implications.
Prior to the pandemic, Medicare reimbursed telehealth services when they were administered at qualifying originating sites (e.g., practitioner office, hospital, rural health clinic) and located in rural areas (geographic site requirements). However, the Coronavirus Preparedness and Response Supplemental Appropriations Act passed by Congress in 2020, permitted the waiver of the originating site requirements during the emergency period. Additionally, the Coronavirus Aid, Relief, and Economic Security (CARES) Act provided the Secretary of Health and Human Services (HHS) the authority to waive the statutory requirements related to Medicare coverage of telehealth services during the public health emergency (PHE). Key waivers necessary to allow for the proliferation of telehealth are set to expire five months after the close of the PHE. Given the impending expiration action by Congress and CMS, it is necessary to ensure that patients can permanently access care provided virtually. As of July 2022, the House passed the Advancing Telehealth Beyond COVID-19 Act (H.R. 4040) to extend COVID telehealth flexibilities in the Medicare program through the end of 2024. Despite a crowded legislative calendar, inclusion of a telehealth bill in a larger end-of-year legislative package is a possibility.
2019-2020 Medicare Beneficiary Telehealth Utilization Analysis
To understand which patient groups have been using telehealth, we estimated the total number of unique beneficiaries and patient days when a Medicare FFS beneficiary received care for one or more services provided via telehealth using the CMS 5% Medicare carrier (physician) and outpatient limited data set (LDS) standard analytic files for 2019 and 2020. Physician and outpatient claims were defined as telehealth if they contained a place-of-service code or modifier for telehealth, or a Healthcare Common Procedure Coding System (HCPCS) that expanded beneficiary access via phone, video, or the internet. We also analyzed pre-pandemic emergency room and inpatient claim diagnoses among unique Medicare beneficiaries using the 5% Medicare outpatient and inpatient LDS files. Broadband access at the county level was determined using American Community Survey (ACS) 2020 data. Since our Medicare claims analyses were derived from a 5% sample of Medicare FFS beneficiaries, our estimates are extrapolated by a factor of 20 to represent 100% of the Medicare FFS population. Our analysis represents 32 million Medicare fee-for-service beneficiaries, with demographic information available for this population in the Appendix. Although there were no clear relationships in telehealth use by age, our analysis did find that 47% of females had at least one telehealth encounter in 2020 compared to only 41% of males.
Medicare Beneficiaries with Higher ER Utilization Are More Likely to Use Telehealth
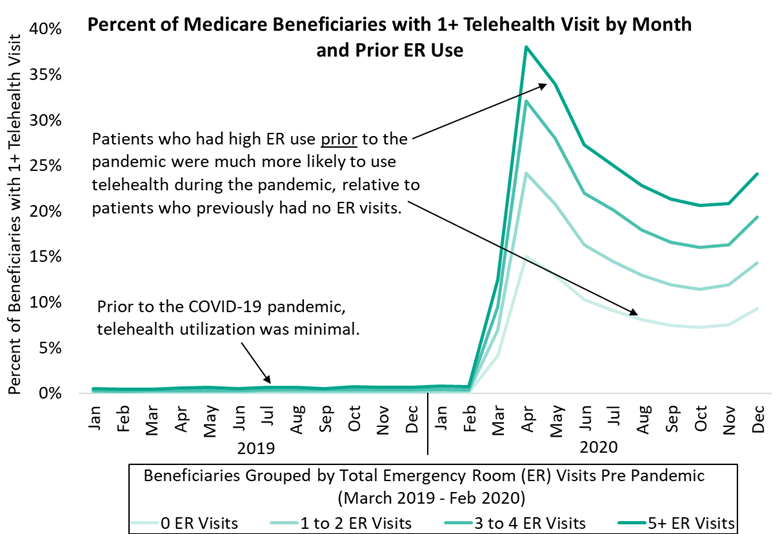
Beneficiaries with the highest emergency room use prior to the pandemic were more likely to use telehealth in 2020. As shown in Figure 1, among Medicare beneficiaries with five or more ER visits between March 2019 through February 2020 (the 12 months prior to the PHE), 38% had a telehealth visit during April 2020, compared to only 15% of beneficiaries who had zero ER visits in the same 12-month period prior to the PHE. Telehealth provided these patients with an opportunity to safely meet with their doctor at a time when there was great uncertainty over the safety of in-person visits.
The number of unique beneficiaries accessing telehealth each month began to decline as more beneficiaries pursued in-person care from July through the end of the year. As more beneficiaries returned to in-person care, telehealth continued to play a vital role for patients that historically had high ER use. Among patients who had five or more ER visits in the year prior to the pandemic, 24% had at least one telehealth visit in December of 2020, compared to just 9% who had no ER visits in the year prior to the pandemic.
Figure 1. Percent of Medicare FFS Beneficiaries With 1+ Telehealth Encounter in March/April 2020 and December 2020 by Prior ER Use
*There was a statistically significant association between telehealth use and emergency room visits pre pandemic (Χ2(3) = 14,538, p < .0001). Chi-squared test based performed for the month of December 2020, using a 5% sample of Medicare FFS beneficiaries.
Medicare Beneficiaries with Chronic Conditions Are More Likely to Use Telehealth
Medicare beneficiaries with certain chronic health conditions were much more likely to adopt telehealth at the start of the PHE. Although only 20% of Medicare beneficiaries relied on telehealth during March or April of 2020, 44% of patients with a prior diagnosis for chronic pain syndrome used telehealth during the same two-month period, as shown in Table 1. Telehealth played an important role in expanding access to medical care for a substantial portion of Medicare patients with health conditions requiring continuous medical care.
Table 1. Percent of Medicare FFS Beneficiaries that used Telehealth by prior Diagnosis
| Among Beneficiaries With a Diagnosis Between March 2019 – February 2020 for: |
ICD-10-CM | % of Medicare Beneficiaries That Used Telehealth in March/April 2020 |
| Chronic pain syndrome | G894 | 44% |
| Major depressive disorder, recurrent, moderate | F331 | 43% |
| Fibromyalgia | M797 | 42% |
| Generalized anxiety disorder | F411 | 38% |
| Sleep apnea, unspecified | G4730 | 37% |
| Chronic diastolic (congestive) heart failure | I5032 | 37% |
| Pulmonary hypertension, unspecified | I2720 | 35% |
| Type 2 diabetes mellitus with diabetic chronic kidney disease | E1122 | 35% |
| Chronic kidney disease, unspecified | N189 | 34% |
| Chronic obstructive pulmonary disease, unspecified | J449 | 32% |
As was the case at the start of the PHE, telehealth use in December of 2020 was common among patients with major depressive disorder, chronic pain syndrome, fibromyalgia, and generalized anxiety disorder, where one in four relied on telehealth (descriptive table not shown). These findings suggest telehealth continues to be a valuable tool for Medicare patients, especially for those with diagnoses for chronic pain and many other conditions.
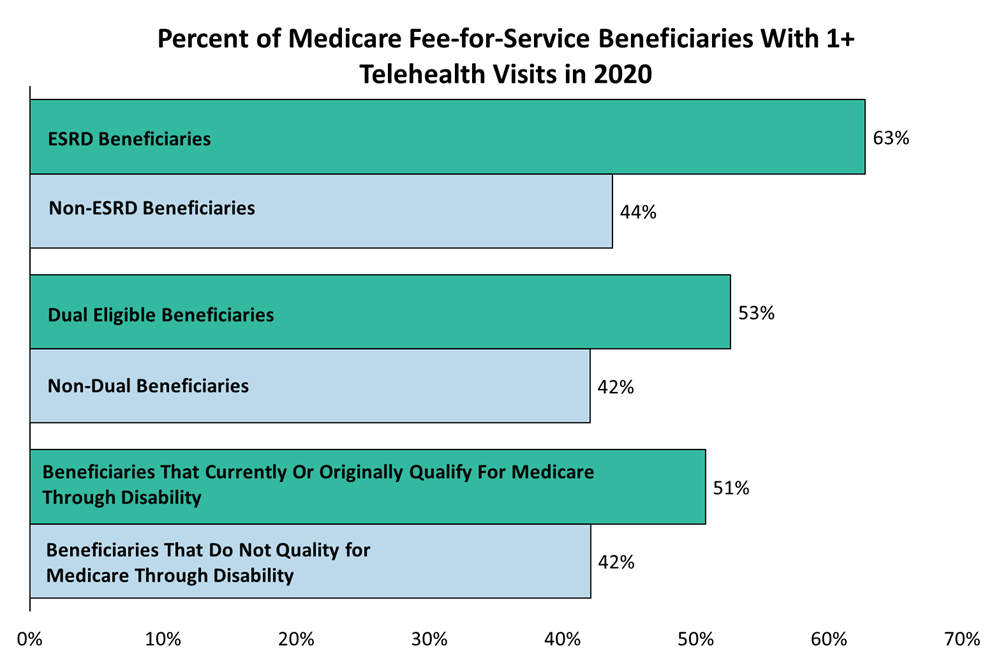
Telehealth Flexibilities Are Key for ESRD and Dual Eligible Patients
Medicare beneficiaries with End Stage Renal Disease (ESRD), dual-eligible, and those who originally or currently qualify for Medicare through disability, strongly relied on telehealth visits during 2020. The share of Medicare beneficiaries with at least one telehealth visit among these patient groups is substantially larger compared to their larger Medicare population counterparts, as shown in Figure 2.
Figure 2. Percent of Medicare FFS Beneficiaries with at least one Telehealth Visit by Beneficiary Group
*Differences are statically significant among groups, ESRD (Χ2(1) = 2,789, p < .0001), Dual (Χ2(1) = 10,841, p < .0001), Disability (Χ2(1) = 8,277, p < .0001). Chi-squared test based on a 5% sample of Medicare FFS beneficiaries.
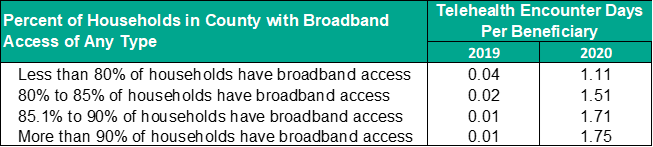
Expanding Broadband Could Further Improve Access to Telehealth Services
Over 10 million Medicare FFS beneficiaries reside in counties where less than 80% of households have broadband access, underscoring the need to improve broadband access. Telehealth use prior to the pandemic was more common in areas with limited broadband access, most likely due to originating and geographic site restrictions which limited telehealth use to primarily rural areas. Telehealth use increased for Medicare beneficiaries living in counties where less than 80% of the population has access to broadband, from 0.04 telehealth encounter days per beneficiary in 2019 to 1.11 in 2020. Telehealth use increased at a much higher rate during the pandemic for counties with stronger broadband access, most likely due to the waiving of geographic and originating site requirements. Although counties with limited broadband access had lower rates of telehealth in 2020 compared to counties with high broadband access, beneficiaries in areas with limited broadband access continued to benefit from telehealth.
Table 2. Telehealth Encounter Days per Medicare FFS Beneficiary by Broadband Access
Telehealth Is Changing Healthcare and the Policy Landscape
Indicated by this analysis, uptake of telehealth delivery did not meet its potential prior to the pandemic. Through the pandemic, we saw systems and infrastructure in place to support telehealth services at levels previously unseen. [5] Aided by legislative and regulatory fast-track changes, providers and patients were able to subvert traditional challenges and pre-COVID barriers, including originating site and geographic requirements.
CMS also added several qualifying telehealth services for the duration of the PHE. Established in the CY 2021 Medicare Physician Fee Schedule (MPFS) final rule, CMS provided coverage for more than 100 services in the Medicare Telehealth List on a temporary (Category 3) basis to last until the end of the PHE. CMS then extended coverage for these Category 3 services through the end of CY 2023 through the 2022 MPFS final rule. The originating site and geographic restrictions, however, will apply to these extended telehealth services for five months after the PHE ends. Congressional action therefore is the only way to permanently revise the originating site requirements and the other barriers to Medicare reimbursement of telehealth services.
As noted previously, CMS provided flexibilities around the originating site and geographic site, which refer to the location of the beneficiary at the time the service is provided. Pre-COVID statute restricts the delivery of telehealth services to certain rural areas of the country (geographic site restrictions) and certain physical locations such as hospitals and physicians’ offices (originating site restrictions). During COVID-19, Medicare and many Medicaid programs expanded coverage so providers may deliver telehealth services to patients in their homes and other locations and in any area of the country. Continuing these flexibilities after the close of the public health emergency may better allow traditionally underserved patient populations to receive care from providers that may be geographically distant. [6]
Public perception of telehealth is improving with patients and providers expressing interest.[7],[8] A literature review found that telehealth is commonly associated with patients being satisfied or highly satisfied with telehealth. Investment in virtual health is increasing.[9],[10] One report estimates that $250 billion of U.S. healthcare spend could shift to virtually enabled care.[11] Under pre-pandemic geographic site restrictions, only two of every 100 Medicare beneficiaries live in counties eligible to receive telehealth services.[12] Through telehealth, there is an opportunity to achieve shared goals of equitable care and improved access. As the nation faces workforce shortages for healthcare providers, telehealth provides a promising pathway to address these provider shortages, particularly by addressing geographic and originating site flexibilities. To preserve access, it’s important that Congress consider proposals to extend telehealth flexibilities beyond the PHE.
Appendix
Table 1. Beneficiary Demographics
| Demographics | N (%) |
| Total | 32,279,317 (100) |
| Age | |
| Under age 65 | 5,292,128 (16) |
| Age 65 to 74 | 15,445,643 (48) |
| Age 75 and older | 11,541,545 (36) |
| Sex | |
| Male | 17,632,670 (55) |
| Female | 14,646,647 (45) |
| Race | |
| Asian | 729,598 (2) |
| Black | 2,839,098 (9) |
| Hispanic | 736,755 (2) |
| North American Native | 183,002 (1) |
| Other | 547,342 (2) |
| Unknown | 787,158 (2) |
| White | 26,456,363 (82) |
| % Of Patients by Total Telehealth Encounter Days in 2020 | |
| Zero | 18,085,245 (56) |
| One to Two | 8,801,940 (27) |
| Three to Four | 2,739,708 (8) |
| Five or More | 2,652,423 (8) |
References
[1] Tsai TC, Jacobson BH, Jha AK. American Hospital Capacity And Projected Need for COVID-19 Patient Care. Health Aff Forefront. 2020. doi: 10.1377/hblog20200317.457910.
[2] Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, Ahmaro IY, Khalid ET, Jumaah FM, Albahri OS, Zaidan AA. Telehealth utilization during the Covid-19 pandemic: A systematic review. Comput Biol Med. 2021 Nov 1;138:104878.
[3] Hamadi HY, Zhao M, Haley DR, Dunn A, Paryani S, Spaulding A. Medicare and telehealth: The impact of COVID‐19 pandemic. J Eval Clin Pract. 2022 Feb;28(1):43-8.
[4] Maese JR, Seminara D, Shah Z, Szerszen A. Perspective: What a Difference a Disaster Makes: The Telehealth Revolution in the Age of COVID-19 Pandemic. Am J Med Qual. 2020 Sep;35(5):429-31. .
[5] Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post‐COVID era. Milbank Q. 2021 Jun;99(2):340-68.
[6] Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L. Assessment of patient preferences for telehealth in post–COVID-19 pandemic health care. JAMA Netw Open. 2021 Dec 1;4(12):e2136405-.
[7] Holtz BE. Patients Perceptions of Telemedicine Visits Before and After the Coronavirus Disease 2019 Pandemic. Telemedicine and e-Health. 2021;27(1). https://doi.org/10.1089/tmj.2020.0168.
[8] Devitt M. Survey, FP Expert Agree: Interest in Telehealth on the Rise. AAFP News. 2019. Accessed from: https://www.aafp.org/news/practice-professional-issues/20190514telehealth.html.
[9] Kruse CS, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7:e016242. doi:10.1136/bmjopen-2017-016242.
[10] Krasniansky A, Zweig M, Evans B. H1 2021 digital health funding: Another blockbuster year…in six months. Rock Health. 2021. Accessed from: https://rockhealth.com/insights/h1-2021-digital-health-funding-another-blockbuster-year-in-six-months/.
[11] Bestsennyy O, et al. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company. 2021. Accessed from: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality.
[12] Partnership to Advance Virtual Care. Response to U.S. Senate Committee on Finance Request for Information (RFI) Regarding Bipartisan Behavioral Health Care Legislation [letter]. 2021. Accessed from: https://www.finance.senate.gov/imo/media/doc/PAVC%20Response%20to%20RFI%20on%20Mental%20Health%20-%20November%2010%202021.PDF.