Stephen Lewis, MD, MHCDS, and Bryan Spear, MBA, MHA
Contact: Stephen.lewis1972@gmail.com
What is the message: Deliberate COVID planning must include thoughtful mitigation strategies for predictable surprises. Strategies include understanding capacity and demand, as well as engaging with stakeholders to understand delivery gaps and reopening challenges. What is the evidence? The authors draw upon their experience at relevant medical centers. Timeline: Submitted June 8, 2020; accepted after revisions: August 3, 2020 Cite as: Stephen Lewis, Bryan Spear. 2020. Dealing with Predictable Surprises from COVID-Related Operational Changes. Health Management, Policy and Innovation (HMPI.org), Volume 5, Issue 1, special issue on COVID-19, August 2020
Predictable Surprises
Max Bazerman and Michael Watkins [1] defined the term predictable surprise as the disasters that organizations should see coming. They note organizations routinely fail to take one or more of three key steps in avoiding predictable surprises: recognition, prioritization, and mobilization.
The COVID-19 novel corona virus – and especially the follow up to it — is a predictable surprise. The pandemic abruptly changed healthcare operations as health system leaders prepared for possible hotspots in COVID-19 demand surges. These operational reprioritizations, new social distancing requirements, uncertainties, and significant fear surrounding the virus led to abrupt stoppage in the delivery of a significant proportion of routine healthcare. The pace of change in healthcare delivery also required relatively decentralized decision making, with clinics and services individually determining cancellation, rescheduling, and staffing policies, as well as telehealth practices.
While the pressure from a growing queue of patients eased with the expansion of telehealth, not all patients’ needs can be addressed virtually. Many patients who have specific needs regarding diagnostic testing or chronic condition management face increased acuity. This presents a unique, but predictable, problem when considering planning for the return to “new normal” healthcare delivery operations.
A Framework to View the Problem
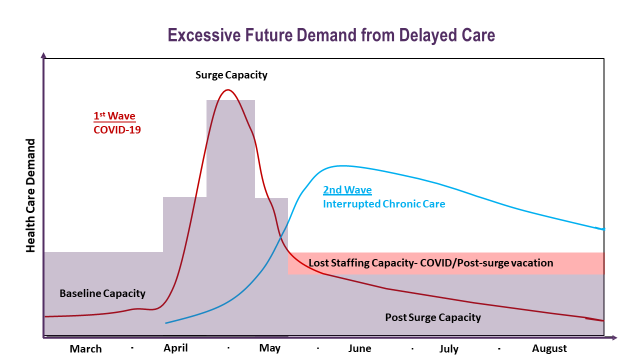
As organizations consider approaches to re-expand direct patient care inside of a new and evolving paradigm for healthcare delivery, key externalities can be easily recognized. Based on the accumulation of patients with delayed care, providers can expect the acuity level of some patients to rise due to a lack of treatment. The figure below depicts a phenomenon in which, while the hospital begins to reopen fully, the system will be stressed beyond its available resources even after the COVID specific patient surge passes.
There are two main elements to understanding this problem.
- Capacity: First is the capacity of the healthcare system post COVID surge. As local restrictions ease, staff will seek and deserve time off to personally recover from the COVID surge which will lower the overall capacity of some services.
- Demand challenges: Second, there will be a rapid demand increase, above the rolling 12-month average, of interdependent services such as referrals, diagnostics, and administrative support. This is attributable to patients with above average acuity re-entering the system first. These patients’ complexity, exacerbated by breaks in continuity of care, may drive above-average requirements for diagnostic testing, referrals, and care management.
These two elements — post-surge decreased staffing capacity plus increased demand — create a predictable surprise for the many hospitals seeking a path forward towards resuming normal operations.
Gathering Data for Solutions
To address this utilization risk, healthcare systems should start at the clinic and service level to understand how they delivered care during the first several weeks of the COVID-19 crisis. It is important to prioritize understanding patient risk stratification approaches, medical service interdependencies, and how virtual health was implemented.
We recognize that only specialists can appropriately risk-stratify their patients. Discussions with these providers suggested global population risk assessment and prioritization was less familiar to specialists. Our observations also indicated significant heterogeneity across the organization in how virtual health was operationalized.
Solving the problem at each institution requires two types of information from key stakeholders within an organization.
- Delivery gaps: First, to capture variation and associated healthcare delivery gaps, senior leaders can send each front-line leader a comprehensive survey with three main sections: Access to Care, Continuity of Care, and Virtual Health.
- Reopening: Second, senior leaders should also present front-line leaders with a series of questions to prepare for reopening, again with three main topics: Staff Reintegration and Capacity Planning; Clinic Operations; and Physical Space Preparation.
The goal is to pair this information with centrally gathered utilization data to tailor operational recovery plans to specific clinic and service needs while creating an integrated global plan.
Looking Forward
Reflecting on our core mission to provide safe, timely, and effective care, we are all preparing to prevent a predictable utilization surprise associated with rapid and variable healthcare delivery operational changes. We should seek a comprehensive coordinated solution built upon customized local solutions that address specific clinical and service differences.
References
[1] Bazerman, M. H., & Watkins, M. (2004). Predictable surprises : the disasters you should have seen coming, and how to prevent them. Boston: Harvard Business School Press.