Lauren M. Bell and Jiayan (Maggie) Chen, Innovation & Strategic Partnerships, Plexxus
Contact: maggie.chen@plexxus.ca
Abstract
What is the message? From the perspective of a shared services organization, the paper discusses some of the challenges in linking procurement to outcomes as a core component of bundled payments relative to the stage of maturity in implementing bundled care in Ontario, the largest province in Canada. Despite the challenges, value-based procurement for specific portions of the bundles is beginning to make a difference in the quality and cost of services in the province. Examples include procuring across the patient continuum to enable bundling implementation for hip and knee patients.
What is the evidence? The authors work with Plexxus, a leading Shared Services Organization in Ontario, which has pioneered value-based procurement for multiple hospitals in the province.
Timeline: Submitted September 11, 2020; accepted after review: September 17, 2020.
Cite as: Lauren Bell and Jiayan (Maggie) Chen. 2021. The Role of Shared Services in Supporting Ontario’s Move to Bundled Care – Understanding the Complexity of Aligning Procurement and Bundled Payments through Value-Based Procurement. Health Management, Policy and Innovation (HMPI.org), Volume 6, Issue 1, Winter 2021.
Bundled Care in Ontario – Background & Current State
Health systems worldwide have been adopting value-based healthcare models to deliver better patient outcomes at the same or lower costs. Ontario, Canada’s most populous province, has also been progressing towards a more value-based healthcare system through the gradual implementation of more integrated care delivery and funding models, commonly known as bundled care. Although bundled care is no longer an entirely new concept in the province, implementation has been incremental and spanning only several patient conditions.
Generally speaking, a fixed payment is allocated for a defined episode of care to a bundle holder who, in turn, works to arrange care for the patient across multiple care settings. This funding model aligns financial incentives with outcomes, promotes care coordination and integration, and improves patient satisfaction. The model also helps to reduce the cost of care by supporting and shifting care to less resource-intensive settings. In the literature, providing care through bundled payments has demonstrated promising results for improving the value of healthcare spending in Ontario and other jurisdictions, such as the U.S. and Netherlands. [1], [2]
Building on the foundation of Quality-Based Procedures (QBPs)[1] and the success of early pilot programs in Ontario, the Ministry of Health (MOH) began implementing bundled care programs at scale during the past couple of years. Since April 2019, a unilateral hip and knee bundle has been implemented across Ontario hospitals that perform joint replacement surgeries. For other bundles such as those that cover shoulder replacement surgeries, Ontario is taking a voluntary and phased approach to implementation due to the complexity of elements such as data collection, reporting, and wanting to assess lessons learned appropriately. [3]
Value-Based Procurement can Support Ontario’s Move to Bundled Care in Helping Purchasers Extract Greater Value from Suppliers and Align around Outcomes
The role of Plexxus
Recent analysis shows that Ontario spends close to 25% of its annual healthcare budget to procure products and services for healthcare providers to deliver patient care. [4] As one of the leading shared services organizations (SSOs) in the province, Plexxus, based in the Greater Toronto Area, focuses on delivering value through service excellence, collaboration, and scalable systems and processes to its 20 member and customer hospitals. Since its inception in 2006, Plexxus has achieved $350 million in savings through its fully integrated supply chain model, inclusive of a scalable digital platform (i.e., SAP) to enable efficient service delivery, advanced decision-making, and analytics.
In addition, Plexxus has significant expertise in complex procurements, with experience across a broad range of categories and competencies, including implementing the first provincial value-based procurement (VBP)[2]of implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy (CRTs) devices. Through applying the principles and practices of VBP, Plexxus has and continues to play a crucial role in successfully leading initiatives that create tangible improvements for hospitals and patients.
The opportunity for bundled care
Bundled care focuses on optimizing care provided across an entire patient pathway rather than individual components of the patient journey in isolation. The episode of care is defined by a best-practice care pathway spanning multiple care settings from hospitals to home and community service providers. By its nature, each pathway relies on both goods and services that SSOs such as Plexxus procure to support the effective delivery of patient care. However, the province’s current procurement model was established with a more sector-based view, where each sector has a very different approach to managing supply chain and procurement of goods and services. This presents a unique opportunity for the province to consider progressive approaches to procurement, such as opportunities to procure for a larger part of the patient pathway to further drive value for patients and purchasers.
Procurements for bundled episodes are a type of VBP that requires a myriad of products and services spanning multiple care settings. By factoring both quality and total cost of patient care into the procurement equation, the new VBP approach focuses on procuring products and services that bring the most value. Value can come in the form of procuring standardized products and services across the continuum of care, which helps narrow unnecessary variation in patient outcomes and drive additional efficiencies through product alignment. [4] For example, when patients move from one healthcare provider to another across a patient pathway, they should be treated with standardized supplies regardless of the care setting unless there is a substantial clinical reason to switch to a different product.
Value might also come from improving the quality of care and patient experience through collaborative purchasing decisions. When an acute care hospital procures medical devices for surgical patients, the hospital should work with their bundle partners, such as home care service providers, to source solutions that include both the devices and home monitoring technology. Compared to the traditional procurement approach driven by the lowest pricing for the surgical devices, the collaborative approach between the healthcare providers across the patient journey has shown to achieve improved patient outcomes and lowered costs for the health system. [4]
Value could also come from fulfilling value propositions for all stakeholders involved in the patient pathway or aligning the procurement to particular outcomes that should be achieved for patients. The provincial value-based procurement of ICDs is not aligned with a bundle but was instead related to procedure-based funding. However, the initiative has delivered value, not only for hospitals but also for patients, providers, and the broader health system by focusing on the importance of battery longevity for patients as an organizing principle. The lessons learned from the initiative, such as comprehensive physician engagement, listening to patients, and early market engagement, are efforts that can be leveraged to support procurement initiatives for bundled care.
The Benefits of Procuring for Outcomes is Clearly Outlined in the Literature; Why has Ontario Struggled to Mobilize this Type of Procurement at Scale?
There is much discussion about the benefits of moving towards procurement activities that consider the larger patient pathway and associated patient outcomes in the literature. However, the empirical evidence on whether procuring for bundled care has delivered on the targeted quality improvement and cost savings objectives remain scant and inconsistent. [5], [6] In this section, a list of challenges is identified with respect to mobilizing procurements to support bundled care from a SSO’s perspective.
Integrated funding policy is still sufficiently in its infancy to allow for the Ontario supply chain to fully address current procurement silos, such as procuring for the entire patient pathway.
Ontario has only touched the tip of the iceberg on implementing bundled payments, in part due to the complexity of payment models for new conditions. The ministry currently supports a diverse funding model that spans a global portion and patient-based funding elements, e.g., quality-based procedures for hospitals. Ontario’s many funding streams do not allow the hospitals to align all their purchasing efforts with the entire episode of care. The funding mechanism for QBPs was developed based on types and quantities of patients treated for a specific acute care procedure. This funding methodology does not contemplate care that might be required throughout the entire episode, such as home and community care. [7]
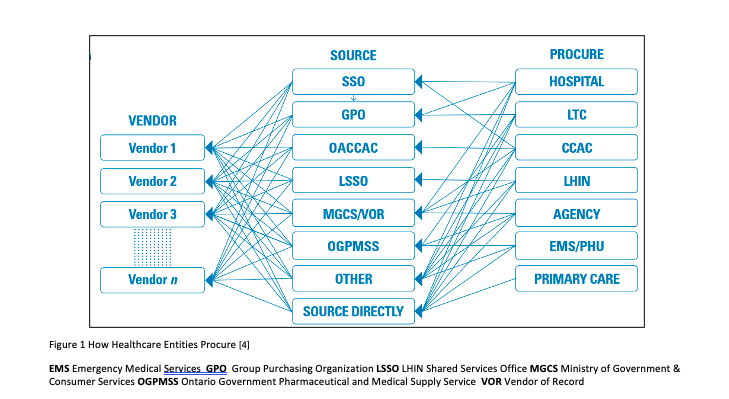
With this in mind, the current procurement model in Ontario has had to remain responsive to the dominant governance and funding structures, which result in highly fragmented and decentralized purchasing decisions. The fragmented decisions are furthered by each care setting — e.g., hospitals, LTC homes, home and community service providers — being supported by their own list of procurement entities.[3](See Figure 1)
Also, there is a diversity of business models within each procurement silo. For example, hospitals can technically procure through a GPO, SSO, government Vendor of Record, and/or their own internal hospital procurement departments. Moreover, procurement continues to operate in response to the dominant funding mechanisms that support more transactional purchasing activities based on annual funding cycles. The procurement approach limits the ability to meaningfully plan for go to market activities that consider a more comprehensive patient pathway and the total cost of care. The siloed funding and fragmented procurement environment have financially incented stakeholders to consider their best interest within a healthcare system that is constantly under financial pressure.
Similar to the mechanism of bundled care, the Ontario government could create an integrated funding policy to enable alignment of the different procurement silos and facilitate more opportunities to consider how to achieve greater financial efficiencies.
It is challenging to measure patient outcomes objectively and tie them to a specific intervention from a vendor. [6], [8]
The success of a VBP is not only measured on purchase price improvements but also defined by achieving value across dimensions that are identified upfront as core value opportunities. Compared to a traditional procurement that focuses on specific requirements and price, it is challenging to define, objectively measure, and fairly evaluate the “value” aspects of a value-based tender. It is even more challenging to reach a consensus on what value is among a wide array of government, health sector stakeholders, and vendors who participated in the VBP initiative.
The basis of a value-based tender evaluation is centered around patient outcomes. Through conversations with vendors, it is evident that they want to provide solutions to improve patient outcomes rather than just providing transactional products and services. However, patient outcomes are usually multi-factorial in a complex patient pathway, making it challenging to attribute any impact of outcomes to a specific vendor solution.
Also, most vendors, unless large consortiums are put in place, cannot be meaningfully embedded in the entire episode of care, making it difficult to deliver much beyond a portion of the patient pathway. Thus, it is often challenging to mobilize a single procurement for the entirety of a bundle, which holds vendors accountable for certain patient outcomes impacting the entire pathway.
When Plexxus engaged vendors on a value-based sourcing initiative, the SSO asked the vendors to propose solutions to improve their product usage on hospital-acquired infection rates. One vendor’s feedback was that any impact on the infection rate could not be directly linked to the performance of their or their competitors’ products. Multiple factors, including the selection of the products, can contribute to variations in the infection rate. Although the real-life example demonstrated the challenge of explicitly tying procurement to outcomes for an acute episode, it is reasonable to believe that procuring for the entire patient pathway could be even more challenging.
Purchasers often have minimal capacity to participate in procuring for the entire patient pathway. [6], [8]
Procurements to support the full bundled episode require a more complex type of value-based procurement. Thus, it requires more time, effort and a more focused contract management approach throughout the life of the agreement to ensure results are being realized. Early and consistent engagement with a substantial number of stakeholders such as healthcare providers, government, and other health system partners is imperative to ensure alignment on the goals and objectives that are being targeted.
More recently, purchasers such as hospitals have had limited clinical capacity to meaningfully invest in VBP relative to patient care and broader health system priorities that the hospitals must also support with already constrained resources. Since the start of the COVID-19 pandemic, Ontario hospitals are facing unprecedented capacity constraints to combat the pandemic. Among other competing demands such as resuming non-essential businesses and elective surgeries, preparing for a potential second surge, and assisting long-term care (LTC) homes, procurement initiatives to support bundled care are a lower priority for hospitals, resulting in many instances of direct negotiations and contracts.
In addition, the inability to procure for the entire patient pathway is not just a result of lacking hospital capacity but also the commitment to collaboration. Hospitals often cannot align for complex procurements due to various operating pressures and not being incented to act collaboratively. It is the hope this will begin to change as the province continues to support the implementation of the recent initiative of Ontario Health Teams.
Moreover, recent McKinsey physician surveys suggest that most respondents still do not have a solid understanding of value-based care or payment models. Thus, 21% of those physicians reported that they would be less likely to participate in those care models. [9] Furthermore, clinicians often want to maintain the status quo compared to exploring complex procurement approaches that can disrupt their usage preferences for specific products. As the role of VBP moves away from enabling clinical preference, increasing physician collaboration involves a significant amount of change management, communication, and strong system leadership from the government.
Examples of Early Wins Achieved from the Value-Based Procurement Initiatives Led by Plexxus
Hip and knee replacement bundles
Despite the challenges discussed in the previous section, several Plexxus hospitals have successfully leveraged procurement as a tool to generate greater value within the post-acute portion of the bundle, such as partnering with community service providers to design more integrated service models. In one instance, a procured home-care service model for hip and knee bundle patients helped ensure a seamless transition for those patients from hospital to home using allied health, nursing support, and virtual care while staying under the funded rate. The participating hospitals and the service provider arranged an up-front agreement on how benefits, both quantitative and qualitative, were measured and evaluated over time.
Key outcome measures for the hip and knee bundles, including readmission and length of stay, were established as the basis for ongoing review of project success. A risk and gain sharing model was also put in place to financially incentivize care collaboration and integration across the patient continuum, enabling bundled care implementation. The model allowed for shared savings between the hospital and the service provider where the direct impact was realized, and penalties if the cost per case exceeded the bundled pricing.
Provincial value-based procurement of implantable cardioverter defibrillators and cardiac resynchronization therapy devices
Even though the value-based procurement for ICDs and CRTs was tied to procedure-based funding, the initiative’s success is the empirical evidence of what a VBP could achieve for Ontario’s healthcare system. The Ministry of Health selected Plexxus to lead the first provincial value-based procurement initiative for ICDs and CRTs. Plexxus worked alongside physician leaders from Ontario’s 12 ICD Implanting Centers, partners, such as CorHealth Ontario and other SSOs, to develop a value-based procurement strategy to increase overall value for patients, and the broader healthcare system. Feedback received from patients such as device longevity, battery life, and MRI compatibility were included as critical considerations for the strategy to improve patient outcomes.
In order to incorporate device longevity into the procurement strategy, a robust longevity analysis methodology was developed to reward longer-lasting cardiac devices that improve patient experience. The approach used evidence-based inputs to support the evaluation of battery longevity. This is critical to moving procurement beyond a short-term decision to focus on the impact to patients over their lifetime. Fewer device replacements are directly related to better patient outcomes and reduced utilization of health system resources.
To support this undertaking, Plexxus established a provincial governance structure to support different elements of decision-making related to the core aspects of the procurement process as well as issues of broader policy and funding. The governance structure brought together clinical, administrative, and health system leadership, supported by a cross-functional team with representation from MOH, CorHealth Ontario, Plexxus, a health economist, and a fairness advisor.
Also, Plexxus developed a multi-phase evaluation approach for clinicians and administrators to meaningfully assess products and services that would address clinical requirements in addition to the hospitals’ business needs. To date, this initiative has demonstrated the benefits of a value-based procurement not only for participating hospitals but also for patients, providers, and the broader health system. It underscores the significant process considerations when designing non-traditional procurements. [10]
Looking Ahead
Ontario’s healthcare system is complex and highly-regulated. Continued efforts to create an environment that can align funding policy with procurement is an important enabler in the transition to a more value-based healthcare system. All healthcare stakeholders, including procurement organizations, aspire to maximize value for Ontario’s health system. However, disincentives and risks inherent from a single-payer system make it difficult for individual stakeholders to achieve better value single-handedly.
The implementation of bundled care will not fully succeed as a transformation activity if the province does not continue implementing integrated funding models at scale. A commitment from the province to scale up bundled care will fundamentally provide additional opportunities for procurement organizations to move away from traditional processes towards more replicable value-based procurement activities. With these building blocks in place, the vendor community can start to accommodate these new approaches by evolving their business models.
Furthermore, Ontario lags behind other jurisdictions when it comes to explicitly incorporating VBP into procurement policy. Ontario’s Broader Public Sector (BPS) Procurement Directive does not explicitly exclude value-based procurement practices. Nonetheless, it lacks clear guidelines to support the implementation of VBP. Through the ongoing evolution of our procurement framework, many stakeholders in the healthcare system could interpret the change in procurement policies as a signal from the government that procurement would eventually be seen as a more formal enabler to the achievement of high-quality care.
For example, the European Union (EU)’s new directive on public procurement encourages the implementation of value-based procurement approaches. [11] The directive also included “most economically advantageous tender” (MEAT) criteria as the procurement guideline for tender evaluation. Contrary to the traditional criteria that are predominately focused on pricing, the MEAT criteria take into account the price-quality ratio while also considering other longer-term costs related to socioeconomic impact and the environment. [11], [12]
In addition to a regulatory environment that supports VBP, a clear government mandate to encourage participation in value-based procurement initiatives is another critical enabler to fully realize the benefits. In the case of ICDs, while a formal mandate was not enacted, the ministry incentivized hospital participation by agreeing to hold funding flat for two years after the contract award. The mandate allows for any efficiencies to be reinvested in the relevant cardiac programs.
As per the structure of all SSOs, Plexxus currently has no direct relationship with the government except through the hospitals they support. As such, the ability to mobilize procurements and provide system leadership that can enable hospital and health sector innovation is often limited. While presently though there are no formal processes for SSOs to table value-based opportunities, Plexxus remains committed to being a strong business partner as Ontario continues its journey to become a more value-based healthcare system. This work will, draw on the organization’s broad supply chain management experience and expertise in value-based procurement.
References
[1] Hellsten E, Sutherland J. Integrated Funding: Connecting the Silos for the Healthcare We Need, C.D. Howe Institute, Commentary No. 463. 2017 January.
[2] Farrell M et al. Impact of Bundled Care in Ontario. International Journal of Integrated Care , 18(S2): A89, pp. 1-8, 2018.
[3] Ministry of Health. Bundled Care (Integrated Funding Models). 2018 April.
<http://www.health.gov.on.ca/en/pro/programs/ecfa/funding/ifm/>
[4] The Healthcare Sector Supply Chain Strategy Expert Panel. Advancing Healthcare in Ontario – Optimizing the Healthcare Supply Chain – A New Model. 2017 May.
[5] Steenhuis S et al. Unraveling the Complexity in the Design and Implementation of Bundled Payments: A Scoping Review of Key Elements from a Payer’s Perspective. The Milbank Quarterly. Vol. 98, No. 1, pp. 197-222.2020.
[6] Zelmer J. Canadian Foundation for Healthcare Improvement. Aligning Outcomes and Spending, Canadian Experiences with Value-based Healthcare.2018 August.
[7] Ministry of Health. Health System Funding Reform. 2015 September.
http://www.health.gov.on.ca/en/pro/programs/ecfa/funding/hs_funding.aspx
[8] Deloitte. How to eat the Value-based Procurement elephant? A Deloitte point of view.
2018 February.
[9] McKinsey & Company. Physician Employment: The Path forward in the COVID-19 era.
2020 July.
[10] Plexxus, Innovation & Strategic Partnerships. ICD Video Series on YouTube. 2019.
<https://www.youtube.com/watch?v=ypHa7Zjv5Pk&list=PL5EE1nUhb-0rAKgSSAGBzo7_aHrlKT4cM>
[11] Gerecke G et al. The Boston Consulting Group. Procurement – The Unexpected Driver of Value- Based HealthCare. 2015 December.
[12] World Economic Forum. Value in Healthcare – Laying the Foundation for Health System Transformation. In Collaboration with the Boston Consulting Group (BCG). 2017 April.
Notes:
[1] Both QBP and bundled care are new funding models introduced by MOH to link funding with quality. Bundled care is an evolved model, expanding on QBP funding methodology, which funds the entire patient pathway and aligns incentives with patient outcomes. QBP is a volume-based payment that aligns with funding for acute care procedures. Also, QBP clinical handbooks were developed by multi-disciplinary expert panels to include metrics, best practices, and evidence-based pathways for select patient populations. Some of the QBP clinical best practice recommendations were used to define the components of patient pathways for bundled care.
[2] VBP is a new procurement approach that incorporates the principles of value-based healthcare. Rather than focusing only on the lowest possible price, VBP focuses on procuring products and services that bring the greatest value to all stakeholders. The value is measured as the best outcomes at the lowest total costs over the full care cycle.
[3] Historically, local health integration networks and community care access centers also had unique procurement requirements, which now have been absorbed by Ontario Health.