Jianhong Wu, Biao Tang, Yanni Xiao, Sanyi Tang, Aria Ahmad, James Orbinski, York University, Xi’an Jiaotong University, and Shaanxi Normal University
Contact: orbinski@yorku.ca
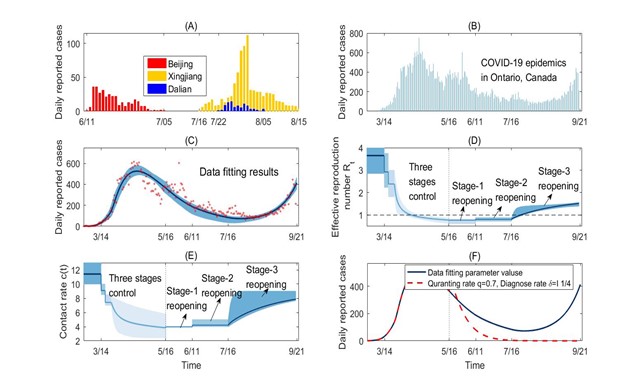
What is the message? Using data from the Canadian province of Ontario (March 12 to September 21, 2020), we model and identify the undesirable cascading effects of premature relaxation of social distancing. When the reproduction rate is near the 1.0 threshold, exponential growth from a large initial pool of SARS-Co-V-2 infections can quickly lead to outbreaks exceeding the contact tracing and testing capacities of public health systems. We then simulate the desirable cascading effects of mitigation interventions that are aimed at quickly reducing the reproduction number well below the 1.0 threshold. This enhancement can bring outbreaks to an end more quickly, and avoiding larger or full scale subsequent waves of transmission. What is the evidence? Using a mathematical model fitted to the Ontario data, we simulated a May 16, 2020 onset in Ontario of an increased quarantine proportion from 40% to 70% and a case detection period shortened from 7.5 to 4 days. With this enhanced testing and contact tracing capacity, the reproduction number would have dropped from 0.78 to 0.3 at the time of Stage 1 reopening. The accelerated rate of case decline across the Province would have ended the first outbreak by the end of June 2020, with a reopening that would have started with a significantly lower number of infections. Timeline: Submitted: December 13, 2020; accepted after revisions: December 16, 2020 Cite as: Jianhong Wu, Biao Tang, Yanni Xiao, Sanyi Tang, Aria Ahmad, James Orbinski. Swift Mitigations and Tipping Point Cascade Effects: Rethinking COVID-19 Control and Prevention Measures to Prevent and Limit Future Outbreaks. Health Management, Policy and Innovation (HMPI.org), volume 5, Issue 1, special issue on COVID-19, 2020.
All Countries are Attempting to Mitigate COVID-19, but with Varying Success
The ongoing COVID-19 pandemic has led to unprecedented mitigation policies designed to identify, contain, control, and prevent outbreaks of SARS-CoV-2 infection. Different jurisdictions have taken different approaches, with varying success. This article contrasts experience with mitigating the pandemic in China and in Ontario, Canada. We suggest strategies that can mitigate the pandemic more quickly and effectively.
Experience in China
Mainland China has achieved successful rapid responses to COVID-19 outbreaks, beginning with the complete lockdown of the first reported outbreak epicenter of Wuhan on January 23, 2020. By February 16, 2020, a month-long, nation-wide lockdown was expanded alongside the four-part “All Policy” – Quarantine All, Collect All, Detect All, Treat All.1 Collectively, these public health measures contributed to mainland China reporting no new cases by March 19, 2020. Following subsequent reopening, local outbreaks in Beijing, Xinjiang and Dalian were reported on June 11, July 7, and July 22, 2020 respectively. Swift lockdowns of provinces with affected cities coupled with expanded contact tracing, access to treatment, and rapid population-wide testing in areas with potential exposure to infection contributed to the success of no new cases in over a month, as shown in Figure 1(A).
When three cases of COVID-19 were confirmed on October 11, 2020 in Qingdao, the city was locked down. The governments’ pre-set scenario goal of immediate contact tracing and immediate testing of the entire Qingdao population (9 million) in five days was exceeded, as more than 10 million samples were collected and tested within four days. With 13 positive cases identified, the city was thereafter reopened. These “swift mitigation’” measures – rapidly reducing contacts followed by intensive contact tracing and widespread population testing —characterize the success of treatment, containment, and prevention in mainland China. From the peak to end of the first and -thus far- only wave of COVID-19 in the country, it took about 45 days. While this specific approach may not be feasible in all regions globally, the experience suggests key elements of a critical problem-solving strategy for subsequent waves of population transmission. Successful approaches need to invoke swift, focused and coherent mitigation interventions that are likely to be more effective than those that are piece-meal, poorly coordinated, and/or ill-timed.
Experience in Ontario, Canada
Modeling social distancing interventions: Initial reductions with risk of recurrence
A similar set of mitigation strategies was employed by governments around the world in their initial response to the first wave of SARS-CoV-2.2,3,4. Taking the Canadian province of Ontario as an example, we modelled a series of escalating social distancing mitigation interventions that were implemented in three consecutive stages between March 14 and May 16, 2020, followed by staggered de-escalation through to September 21, 2020 (Figure 1B). In addition to school closures (Stage 1) and restrictions to public events and recreational venues (Stage 2), the “swift mitigation” measures of shutting down all non-essential workplaces (Stage 3) was essential to reducing the Effective Reproduction Number, below the 1.0 threshold by on or around April 16, 2020.
This trend marked a strong start but was still susceptible to the emergency of new infections. Reflecting the sum effect of all mitigation interventions, when approaches the 1.0 threshold and the number of infections in the population is significant, a subsequent wave of infection is likely to emerge. A new wave is particularly likely where increased social contact allows for broader-based transmission, thereby driving above the 1.0 threshold.
Recurrence: April to September 2020
Using a transmission dynamics model fitted to the daily incidence data in Ontario (Figure 1C), we observed two key trends. First, although decreased to below 1.0 around April 16, 2020, it remained close to this threshold, resulting in only a slow case decline rate. Second, even with the quarantine proportion and case detection rate achieved at the end of Stage 3, can exceed the 1.0 threshold when the contact rate reaches only two-thirds of the normal full rate after reopening. This indeed happened when the province moved to regional de-escalation from Stage 3 on July 16, 2020 allowing businesses and public places in approved regions to re-open with safety and occupational measures in place.
Our estimation shows a gradual increase in the contact rate (Fig. 1E). However, contact tracing coverage and testing capacity remained relatively unchanged, with the quarantine proportion at 38% and a diagnostic testing confirmation period of 7.5 days after infection. As a result, the effective reproduction number gradually increased to 1.5, leading to a second wave in September 2020. In turn, the Province re-imposed modified Stage-2 mitigation measures in some hotspots.
Simulations: What if contact tracing had been higher and testing faster?
Using our model, we simulated a May 16, 2020 onset in Ontario of an increased quarantine proportion from 40% to 70% and a case detection period shortened from 7.5 to 4 days (Figure 1F). With this enhanced testing and contact tracing capacity, would have dropped from 0.78 to 0.30 at the time of Stage 1 reopening. The accelerated rate of case decline across the Province would have ended the first outbreak by the end of June 2020, with a reopening that would have started with a significantly lower number of undetected infections (if any). This would have allowed public health resources to be mobilized for swift and focused responses to any new localized hotspots, and likely avoiding a full-scale second wave of transmission.
In contrast to these desirable cascade effects – where enhanced social distancing measures maintain a low leading to reduced number of new infections, together with swift public health testing and contact tracing – Ontario experienced the undesirable cascade effects of pre-mature relaxation of social distancing. Unfortunately, as a result, the exponential growth from a large initial pool of undetected infections quickly led to outbreaks exceeding testing and tracing capacity. This negative cascade reinforced the resurgence of the pandemic in Ontario.
The power of tipping points: Triggers for a second wave in Ontario?
Stage 1 reopening in Ontario started on May 16, 2020 even as new cases continued to be reported daily, suggesting that may have been hovering around the 1.0 threshold. According to catastrophe theory and dynamic systems bifurcation theory, the province was at a “bifurcation point” with subsequent tipping point cascade effects, when de-escalation of social distancing began on May 16, 2020.
Tipping point cascade effects suggest that while a small increase to the bifurcation parameter (in this case, can trigger a second wave, further reduction of this bifurcation parameter near the tipping point can accelerate an exponential decline in new case transmissions. In Ontario, the number of total and new daily cases was judged to be “small” — wrongly, it appears — in deciding to begin reopening on May 16, 2020. Public health resources were likewise judged to be sufficient, instead of scaling testing, contact tracing, quarantine, and isolation efforts, which would lead to a further decrease of . Hence, the analysis suggests a missed opportunity to prevent the second wave.
Implications for Global Mitigation During the Second Wave
Similar situations globally can be identified on the WHO Coronavirus Disease Dashboard, with countries reporting subsequent waves of transmission with even larger peaks that have imposed significant challenges to public health systems in the face of public fatigue.5 Prolonged lockdowns have become a real possibility in many parts of the world. Yet this time, a critical problem-solving strategy for subsequent waves of COVID-19 population transmission should invoke swift, focused, and coherent mitigation interventions that aim to reduce the effective reproduction number well below the 1.0 threshold. This approach is likely to be more effective than strategies that are piece-meal, poorly coordinated, and ill-timed.
At least two factors have contributed to the occurrence of second waves in many countries. First, SARS-CoV-2 has high transmissibility with a high basic reproduction rate when activities resume.6,7 Second, although most countries implemented a range of public health mitigation interventions, implementation has often been lax and inconsistent, resulting in tipping point cascade effects that lead to further outbreaks.
One important strategy for controlling infectious disease outbreaks is to reduce below the 1.0 threshold. However, it is easy to stop too soon. Given the high transmissibility and reproduction rate of SARS-CoV-2, an effective reproduction number below but near this threshold could result in a prolonged period until the end of the outbreak.
Looking Forward
The global scale of the COVID-19 pandemic has catalyzed to significant advancements in public health interventions, including rapid testing and enhanced contact tracing capacities. With these, the period from peak to end of the second wave can and should be shortened when tipping point cascade effects are fully taken into account.
Effective strategies to confront subsequent waves of outbreaks and to safely reopen from full, staged or localized lockdowns require swift, focused, and coherent mitigation interventions to quickly reduce the effective reproduction number well below the 1.0 threshold. Enhancing public health mitigation efforts at the bifurcation tipping points can further accelerate the decline of new cases, followed by enhanced rapid testing and contact tracing when the case numbers are small.
Figure 1.
- Panel (A) Local outbreaks in Beijing, Xinjiang, and Dalian: shock mitigation and rapid testing enabled quick control8.
- Panel (B)-(F) COVID-19 epidemic in Ontario, Canada from Feb 26 to Sep 21, 2020. Here, the model by Biao et al.9 is used to evaluate the contact rates, diagnosis rate, and quarantine proportions, following the timelines of three stages of social distancing escalation to control the 1st wave, and the three stages of reopening. Social distancing de-escalation led Ontario to reopen on May 11. In our simulation (Fig 1F), with the quarantine proportion increased from 38% to 70% and diagnosis period shortened from 7.5 to 4 days starting on May 16, the reproduction number would have decreased with an accelerated rate of decline, such that the first outbreak would have ended by the end of June and the reopening would have started with very small number of infections. Public health resources could then have been mobilized for swift reaction to any new local hotspot to avoid a full scale second wave. In contrast to this desirable cascading effect — contact reduction leads to a small number of new infections and enables swift public health tracing and testing — Ontario experienced the undesirable cascading effects of relaxation of social distancing too early, such that the exponential growth from a large initial pool of infections quickly led to outbreaks exceeding the tracing and testing capacity.
Author detail: Jianhong Wu1,3,†, Biao Tang2,4,†, Yanni Xiao2,4, Sanyi Tang5, Aria Ahmad,6 James Orbinski6
1 Laboratory for Industrial and Applied Mathematics, Department of Mathematics and Statistics, York University, Toronto, Canada
2 Interdisciplinary Research Center for Mathematics and Life Sciences, Xi’an Jiaotong University, China
3 Fields-CQAM Laboratory of Mathematics for Public Health, York University, Toronto, Canada
4 School of Mathematics and Statistics, Xi’an Jiaotong University, Xi’an, China
5 School of Mathematics and Information Science, Shaanxi Normal University, Xi’an, China
6 Dahdaleh Institute for Global Health Research, York University, Toronto, Canada
† The two authors contributed equally
Author contributions: Conceptualization, J.W., B.T. and J.O.; validation and simulation, B.T.; data curation, B.T.; writing—original draft preparation, B.T., Y.X., and S.T.; writing—review and editing, J.W., B.T., and J.O.; All authors have read and agreed to the published version of the manuscript.
Funding: This research was funded by the Canadian Institute of Health Research (CIHR) 2019 Novel Coronavirus (COVID-19) rapid research program, the Canada Research Chair Program and the Natural Sciences and Engineering Research Council of Canada (JW), and the National Natural Science Foundation of China (grant numbers: 11631012 (YX, ST), 61772017, 12031010 (ST)).
Competing interests: The authors declare no competing interests.
References
- Xiao et al., Linking key intervention timing to rapid decline of the COVID-19 effective reproductive number to quantify lessons from mainland China, Int. J. Infect. Dis. 97, 296-298 (2020).
- S, Hsiang et al., The effect of large-scale anti-contagion policies on the COVID-19 pandemic, Nature, 584, 262–267 (2020).
- Tian et al., An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China, Science, 368, 638-642 (2020).
- J. Kucharski et al., Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study, Lancet Infect. Dis. 20(10), 1151-1160 (2020).
- WHO Coronavirus Disease (COVID-19) Dashboard, https://covid19.who.int/table. [Accessed at Oct 15, 2020].
- Sanche et al., High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg. Infect. Dis. 26(7), 1470-1477 (2020).
- Flaxman et al., Report 13: Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries.
- National Health Commission of the People’s Republic of China, http://www.nhc.gov.cn/xcs/yqfkdt/gzbd_index.shtml [Accessed on Oct. 26].
- Tang et al., De-escalation by reversing the escalation with a stronger synergistic package of contact tracing, quarantine, isolation and personal protection: Feasibility of preventing a covid-19 rebound in Ontario, Canada, as a case study. Biology 9(5), 100 (2020).