Hoyt Gong and Cecilia Wang, The Wharton School, University of Pennsylvania
Contact: hoytgong@wharton.upenn.edu | yixiwang@wharton.upenn.edu
Abstract
Lead Sentence: China’s emergency response system at the initial outbreak of COVID-19 left unintended fallout effects on non-COVID-19 patients as medical resources were rationed early in the pandemic.
What is the message? China’s emergency response system at the initial outbreak of COVID-19 left unintended fallout effects on non-COVID-19 patients as medical resources were rationed early in the pandemic. The authors scope the fallout impact on affected patients via a quantitative case study on kidney dialysis, confirm similar challenges with perspectives from Wuhan healthcare providers, and corroborate healthcare access scarcity sentiments among a general Chinese population. While these issues have been addressed over time as the health system has adjusted, the authors provide structural, cultural, and systematic recommendations that highlight ways of solving the problems earlier when similar challenges arise in the future. Opportunities include early precision risk measuring interventions, widespread federal telemedicine adoption, strategic plans to allocate medical resources in times of infectious disease outbreaks, and stakeholder collaboration to enable natural mutual aid and prioritized national health.
What is the evidence? Interviews with physicians and nurses in Wuhan (N=7), WeChat and Weibo patient study survey data (N=162 across 24 provinces), and authors’ implications drawn from analysis of early COVID-19 articles in China. The evidence was collected from February to March 2020, and the results were analyzed during April to May 2020.
Timeline: Submitted November 2, 2020; accepted after revision: December 10, 2020.
Cite as: Hoyt Gong and Cecilia Wang. 2021. China COVID-19 Fallout Effects: An Analysis of Emergency Response to non-COVID needs. Health Management, Policy and Innovation (hmpi.org), Volume 6, Issue 1, Winter 2021.
Early in the Pandemic, China Faced Challenges in Responding to non-COVID Medical Needs
As Wuhan’s Hubei province went on lockdown in January 2020, early Chinese media coverage captured the frontline COVID-19 response that would shortly emerge as a global pandemic. With unprecedented pace of usage, medical resources ran scarce and emergency response measures were placed across hospitals nation-wide for rationing. Scarcity in PPE, healthcare personnel, and delivery capacity led to fallout effects in other health departments as concentrated attention was placed on the COVID-19 response. We define fallout effects as constraints impeding ill, non-COVID-19 patients from seeking proper care.
This article explores the impact of the pandemic’s fallout effects on China’s non-COVID-19 sick population early in the pandemic, taking varying healthcare stakeholder perspectives and evaluating gaps in China’s existing emergency response system in the early emergence of COVID-19. To address these challenge gaps, the authors offer suggestions for China’s federal emergency response to prepare and respond quickly to future disease outbreaks.
A Three-part Study
This study was conducted starting from January through March 2020 at the peak first onset of COVID-19 in China. The key stakeholders addressed in this study were Chinese healthcare providers (physicians and nurses), Chinese citizens across varying general health status, and Chinese kidney dialysis patients. The following sections illustrate each study data component with methodology and results of analysis. We discuss a dialysis case study, interviews with healthcare providers, and an online survey.
Dialysis Case Study
The fallout effects of COVID-19 gained visibility early in the pandemic with stories in Wuhan such as that of nurse Zhang Qin and her late father who passed away in late January. Qin’s father suffered from long-term uremia that requires dialysis at hospitals three times per week. However, immediately when Wuhan closed, the city’s hospitals stopped providing many medical services to prevent the risk of intra-hospital transmission, including the dialysis that Qin’s father required. After being denied transfers to two other hospitals, Qin’s father passed away at home days later due to the lack of dialysis treatment.
“I was busy saving others, but I can’t save you. I am sorry and I love you so much, Dad.” —Nurse Zhang Qin
Caught in the pandemic response, Nurse Qin was brought to the frontlines in a Wuhan hospital working 10+ hour days every day without time off and was unable to help her father. Medical resource allocation heavily led to fallout damage in chronic disease, particular in this case of dialysis.
Following many heartbreaking stories, the authors provided an estimate of the number of dialysis patients that could be affected by the reallocation of resources in the hospitals. From the Chinese Society of Nephrology, there are currently 100 million people in China suffering from chronic kidney disease (CKD), with 1 million of them having end-stage renal disease (ESRD)1. These one million patients would require regular dialysis to sustain their lives. It is estimated that only about half of these patients receive their dialysis regularly, due to lack of appropriate facilities and education in many areas. By multiplying 50% to the total number of ESRD patients, Chinese Society of Nephrology concluded that at least 500,000 patients in China undergo regular dialysis.
Since no provincial-level dialysis statistics were publicly available, the authors decided to estimate the number of dialysis patients in Hubei Province using its demographics data. Hubei Province is a densely populated region, accounting for 4% of the national population. Assuming an equal distribution of dialysis patients, there would be 500,000 * 4% = 20,000 patients receiving regular dialysis in Hubei Province. Taking a conservative approach, the authors assumed that half of the dialysis patients in Hubei Province were affected, which brought us to a total of 20,000 * 50% = 10,000 affected dialysis patients.
The dialysis patients were denied access to care for several reasons. First, some hospitals were designated to treat only COVID patients and extremely emergent patients. This means that they shut down operations for many departments, including the dialysis centers within the hospitals. Second, patients and their families were afraid to enter the hospitals because of the concerns about potential infections. This point is further substantiated by the survey data below. Additionally, since the transportation was shut down between Wuhan and many neighboring cities and towns, patients who needed to travel to a different community to receive their dialysis now lost their channel.
The estimate of 10,000 affected dialysis patients is conservative. The actual number of patients could be even higher. Furthermore, there remained many other types of chronic patients, such as patients with cancer, HIV-AIDS, or cardiovascular diseases. These patients were likely to be affected by the same reason—that the hospitals relocated their resources to concentrate on COVID, leaving behind the non-COVID patients. Together, the number of affected chronic non-COVID patients in Hubei Province was high, shedding light into the fallout effects of COVID-19 in the earlier stages of the outbreak.
Interviews with Healthcare Providers
The authors conducted seven primary interviews with frontline physicians and nurses in hospitals within Wuhan, Hubei. All healthcare providers asked to stay anonymous The interviews were conducted in Chinese and the scripts of the responses were translated into English later. There were some barriers to finding enough interviewees, since many healthcare providers were either too busy at the time or unwilling to share their opinions on this controversial matter.
There were five main questions asked to each of the interviewees with regard to hospital operations, resource allocations, and emergency preparations. Across the board, the responses were similar and key illustrative information is recorded below. Note that each letter represents a different respondent, and the letter is not indicative of any identity of the interviewee.
- How many patients were in your department on a regular day vs. during COVID period?
A: “175 patients on a usual day, but only 2-3 patients per day now.”
B: “There are 11 wards in our department and only 2 of them are open now. It will be only one ward opening as of tomorrow.”
- How much medical resources have been deployed to treat COVID patients?
C: “More than 90% of nurses in our department and about 50% of doctors from unrelated departments were called to the frontline hospitals.”
D: “All outpatient departments were closed and all resources were sent to the Fever Clinic, Department of Infectious Diseases, and ICU.”
- How can patients with chronic diseases get appropriate treatment during this period?
A: “There is a severe lack of prescription drugs and even I myself, still working at the hospital now, can’t get my antihypertensive drugs.”
B: “Many patients living outside of Wuhan will seek medical care in Wuhan. However, with the strict lockdown policy, none of them was able to do that these days.”
E: “The oncology department has been used to receive and treat COVID-19 patients now. There are an estimate of 1000 hospital beds there and all the cancer patients have to go home.”
F: “I know there are 18 patients left in the Gastroenterology department as of today. For most departments, there will be a max of around 10 patients and a min of 2 to 3 patients.”
- What preventative measures were in place to minimize the risk of COVID infection in the hospital?
D: “Every patient going into the hospital needs to be checked with body temperatures and travel histories. There is a strict division between the COVID-19 section and the rest of the hospital.”
G: “The best preventative measure is not having people being in the hospital. Since most parts of the hospital were closed now, few patients actually come. It requires too much time and effort to confirm if someone is 100% COVID-negative. If they did come to the hospital, it may be a danger to other patients and physicians.”
- Does the hospital still treat emergent situations?
B: “The emergency department is still open, although only half the regular staff still work there. However, we have many fewer cases on average in the past two months because people just stayed at home.”
E: “The emergency department is still open but we cannot operate on any patients now. I had someone reaching out to me saying he cut his finger at work, but I can’t operate on him in the hospital. We just don’t have any anesthetists now.”
G: “Patients who arrive at the Emergency department are in much worse condition on average. People don’t want to show up to hospitals during this particular time unless it’s life-threatening.”
To summarize, healthcare providers generally agreed that the normal hospital operations were greatly affected and most resources were dedicated to COVID patients. This shift had a substantial impact on the non-COVID patients, especially chronic patients who need to go to the hospitals on a regular basis. There seemed to be a lesser impact on the emergent patients, although limitations still existed for patients who require surgeries and more complicated procedures.
Online Survey Data
The authors created and distributed an anonymous digital survey2 to Chinese citizens via the online platforms WeiBo and WeChat as the main mediums for outreach. The data collection period lasted for one month (February 2020 – March 2020) and the 163 survey respondents represented 24 Chinese provinces. The full questionnaire is referenced in the appendix.
The key results of the survey fall into three categories of respondents’ experiences with (1) drug shortages, (2) chronic disease, and (3) acute illness.
- Drug Shortages
As an aggregate, 10% of respondents noted they experienced drug shortage challenges, defined as a lack of pharmaceutical medication due to access constraints imposed as a fallout effect of COVID-19 response. Of this group, more than half (56%) said they were not using the available government online drug platform3. Survey results show that this lack of use was largely attributed to an absence of awareness that such a federal pharmaceutical repository exists. On average, four out of five Chinese citizens experiencing drug shortage issues that did not utilize the People’s Republic of China (PRC) national program did so only due to a lack of information about the program’s existence.
- Chronic Disease
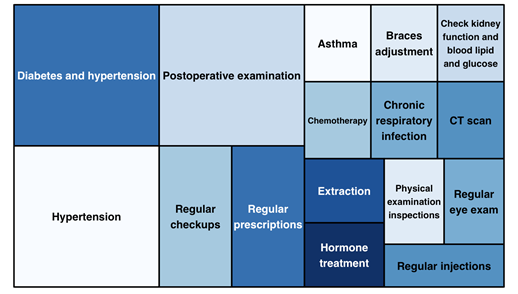
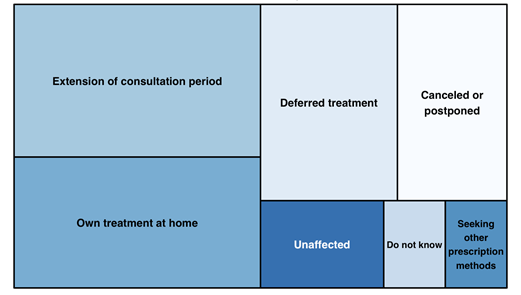
Respondents were asked about their health status with regards to having some form of chronic disease that requires regular medication or hospital treatment. 20% of respondents (27 people) reported having such a condition, but only 37% of this group (10 people) were able to still seek care from their standard provider. The rest were unable to access hospitals for their chronic disease. These respondents further reported the chronic issues they faced and how they coped with the lack of access in Figures 1 and 2 below.
Figure 1: Proportional mapping of respondents facing chronic disease
Figure 2: Proportional mapping of how chronic disease patients adapted to lack of access
- Acute Illness
The final survey questions asked respondents to evaluate if they suffered from an acute illness and their resulting experience seeking medical care. Notably, of the 23 respondents who self-reported an acute illness condition, only 6 of these individuals (24%) chose to seek care in a hospital setting. These patients who were still able to attend reported that their quality of healthcare delivered was almost as high as prior to COVID, with a median 4.25 of 5 compared to pre-COVID-19 quality of care.
Hence while we observe that most acute illness patients were unable to seek care due to fallout effects, a minority of manageable patient acute illness cases were accepted. China’s hospitals in early COVID-19 days focused on tight triaging measures, maintaining relatively standard quality of care at the cost of turning away a majority of other patients.
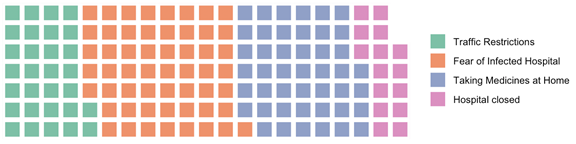
Of the remaining 76% of acute illness patients who were unable to access hospitals for treatment, the breakdown for their rationale is described in Figure 3 below. These patients each reported multiple challenges towards their inability to access care, falling into four categories (listed in order of complaint frequency): (a) fear of infection from hospitals admitting COVID-19 patients, (b) resorting to taking at-home and community-sourced Western and Eastern medications, (c) physical traffic restriction barriers preventing transportation to hospitals, and (d) physical hospital closures.
Figure 3: Rationale breakdown of acute illness respondents’ lack of medical access
Recommendations
Our early analyses demonstrate gaps that emerged in non-COVID-19 patient care across Chinese patients and providers during early stages of the pandemic. While these fallout effects have been mitigated with China’s COVID-19 recovery that has phased in at the time of this manuscript’s delivery in late 2020, the early challenges can serve as lessons learned for future disease outbreak response efforts by the PRC. We describe the key takeaways for application towards a future preparedness and emergency response in China based on the study components.
Structural Recommendations
Enable precise risk identification interventions through early federal sponsorship: An early federal response via financing existing health technologies alone will not adequately respond to pandemic effects on all healthcare departments. The emergence of precision health and patient risk stratification modalities (e.g., contact tracing, health data collection) supports the structural ability to target resource delivery for at-risk groups that may otherwise be overlooked in the midst of a pandemic response. By identifying at-risk and infected patients, the Chinese government is able to target precise healthcare delivery information to specific populations, such as the PRC’s pharmacy delivery program for chronic disease patients and city road closures for at-risk patients within a hospital’s catchment area. China’s status as a one party dominant governing system and widespread Citizen adoption of multipurpose super apps such as WeChat uniquely positions the PRC to enable rapid precision health interventions acting on patient risk data.
Build widespread telemedicine capabilities that encourage rapid standard of care adoption: Capacity building in the wake of contagious (historically R0 > 1.5) disease spread requires an emphasis on remote telemedicine services and contained treatment facilities. To encourage a more resilient Chinese health system, PRC can emphasize adoption of digital telemedicine services (e.g., virtual health platforms; PRC’s pharmacy delivery fulfillment program) across provinces to drive rapid systematic adoption of the new standard of care.
Cultural Recommendations
Encouraging community self-mobilization as a positive step of natural mutual aid: The emergence of online communities such as WeChat groups that provide medical advice and hands-free medications to its chat members highlight the natural mutual aid that emerges within the community. This self-mobilization of Chinese citizens created spaces in the informal sector in which community support gave benefit to their health outcomes. The PRC has the ability to amplify the successes of these informal communities by nationally acknowledging and advocating natural mutual aid as positive grassroots endeavors.
PRC collaboration with many representative hospital units in provisioning greater medical authority: While the cultural context of China rests on a backdrop as a one party republic with final decision-making authority, there remains an opportunity to shift further decision making autonomy onto medical authorities when facing a national epidemic. Particularly crucial in the early stages of an outbreak, government officials must recognize the expertise lent by medical personnel and defer authority in order to prioritize the national healthcare interest.
Systematic Recommendations
Strategic allocation of medical resources in times of infectious disease outbreaks: One important factor leading to the fallout effects on non-COVID patients is the lack of appropriate medical resources for them. During the initial stages of COVID outbreak, the federal and local government decided to shift the majority of the resources to prevent and treat COVID patients. While this seems to have been effective in containing the COVID spread, non-COVID patients often lacked access to care. The government should prepare strategic plans, learning from the mistakes of this time, that specify clear divisions of resources among emergent vs. regular healthcare operations in times of public health crisis.
Construction of specialized hospitals and more dialysis centers: Most hospitals in China are large, generalized hospitals. The lack of specialized hospitals and certified clinics made it difficult for patients to go to the hospitals during a pandemics period. Patients may be concerned about the risk of infection by going to the hospitals or the lack of doctors in such hospitals. The construction of specialized hospitals can reduce the risks of non-COVID patients going to the hospitals for other healthcare needs. For example, the establishment of more dialysis centers will likely prevent tragedies such as the one that happened to Zhang Qin’s father.
Limitations of the Study
The study has several limitations. First, the primary data collection could face biases and errors. There was no publicly available data on the fallout effects in China given the short amount of time between the outbreak and the research. Second, the authors were not able to speak with as many healthcare providers as hoped given the timeline of the research and the level of sensitivity of the topic. The lack of coverage from some important hospitals in Wuhan may have left out some important aspects of analysis. Third, the survey data may not be an accurate representation of the overall demographics. The sampling bias existed because it is likely that people who encountered relevant problems were more willing to participate in the study than those who did not. Furthermore, most of the survey respondents range from age 20-50 and came from middle income families. It is likely that demographics that experienced more severe fallout effects of COVID, especially within the lower-income population, were not featured by the online survey.
Looking Forward
Our analysis from the case studies on chronic patients, interviews with front line healthcare providers, and a timely online survey all indicated that China’s emergency response system at the initial outbreak of COVID-19 left unintended fallout effects on non-COVID-19 patients. The unbalanced resource allocation towards COVID had corollary effects. Patients lacked access to basic health care services merely because they were not COVID patients, which caused tragic consequences to many patients and their families both in the short and long term.
Fortunately, the PRC recognized the tragic fallout effects and their policy responses adapted to these challenges by late March and early April. With most hospitals reopening for non-COVID patients starting in April, the majority of the observed fallout effects gradually receded. From follow-up discussions with the healthcare providers and some survey respondents who initially participated in this research, the authors concluded that most hospital operations and standard protocols had been restored in the areas studied.
For scholars interested in similar research topics of observing the fallout effects of COVID in different regions, similar methods and channels can be adopted. One leading advantage of the method is the timeliness of analysis. Had the studies been done later in the year, the authors may not have caught as much real-time stories and sentiments toward the government’s initial policy. The ability to identify the problems quickly will facilitate better policy-making and international collaborations to minimize similar risks. It is the hope that this study will help China and the world reflect on the fallout consequences of COVID response and be more prepared for future public health crises.
Appendix 1—Chinese Society of Nephrology
Chinese Society of Nephrology: http://www.csnchina.org/cn/news.asp?id=39.html
Appendix 2—Digital Survey
The digital questionnaire sent out via WeChat and other social media:
Figure 4: Snapshot of the introduction and the first two questions
Appendix 3—Available Online Drug Platform
Starting on February 26th, 2020, the Hubei government has published some online drug platforms on which people can register for the drugs they need and have them delivered. In the meantime, 50 designated pharmacies in Wuhan reopened for patients to pick up prescription drugs, some of which included an online ordering and delivery services.
Announcement from Health Commission of Hubei Province regarding online drug delivery platform, published on Feb 27th, 2020 (website in Chinese):
http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/fkdt/202002/t20200227_2160653.shtml
WeDoctor—the first online drug delivery and consultation services sponsored and supported by the Chinese government following COVID outbreak: https://promo.guahao.com