David Scheinker, Clinical Excellence Research Center, Stanford University, and Roger E. Bohn, Clinical Excellence Research Center, Stanford University, and University of California San Diego
Contact: dscheink@stanford.edu
Abstract
What is the message? Hospitals are facing a growing workforce crisis fueled by staff burnout and less time for patient care as providers spend more of their day interfacing with the time-consuming electronic medical records (EMR). Software as a service (SaaS) has driven significant productivity gains across numerous industries and in hospitals, SaaS is used from revenue management to employee scheduling. Healthcare technology innovation strategies that expand the use of SaaS to both redesign workflows and ensure technical integration with the EMR, could increase productivity and help mitigate workforce challenges.
What is the evidence? The authors analyze existing EMR-integrated decision-support tools and illustrate the benefits of a provider-focused approach.
Timeline: Submitted: , 2022; accepted after review: , 2022.
Cite as: David Scheinker, Roger E. Bohn. 2022. Improving Healthcare Productivity by Using Technology Strategically. Health Management, Policy and Innovation (www.HMPI.org), Volume 7, Issue 3.
Introduction
United States healthcare costs, especially the cost of hospital care, have grown far faster than those of other countries or corresponding improvements in quality.[1] A long-brewing workforce shortage has been exacerbated by the COVID-19 pandemic.[2] Hospitals are facing a workforce crisis, in addition to the perennial problems of “unsustainably” high costs and poor consumer experience. Care providers such as physicians and nurses are trapped in a vicious cycle: burnout increases workforce attrition,[3] attrition and staff turnover leads to more work for those remaining, more work increases stress, and more stress leads to more burnout. The implementation of electronic medical record (EMR) systems have increased care provider documentation burden, aggravated provider burnout, and failed to provide hoped-for productivity gains or to provide interoperability across sites or systems.[4] As a result of reduced productivity and COVID-created demand surges, many hospitals and clinical programs are struggling to maintain access to care while suffering operating losses.
Hospital EMRs often lack basic functions needed to optimize workflows. Single-institution studies of low-value interactions with the EMR (interactions that have been eliminated without impacting patient care or essential documentation), found that these activities can be reduced by more than an hour per 12-hour nurse shift.[5] Specific EMR tasks, such as admitting a patient to a hospital, could be shortened by an average of 30%.[6] In a survey of over 70,000 nurses, about 71% said that the way orders were handled in the EMR impeded patient care, nurse efficiency, or both.[7]
Software as a service (SaaS) companies have driven significant productivity gains across numerous industries. In hospital care, SaaS is available for essentially every other aspect of hospital operations except patient care workflows; SaaS is common for revenue management, data visualization or business intelligence, and staff scheduling. In theory, EMR should improve productivity through enhanced analytics enabling more efficient workflows, and through better patient outcomes. In practice, the difficulties of changing workflows and of integrating new analytics with the EMR are major barriers to achieving this vision. Over the last two decades, academic researchers and technology companies have designed thousands of machine learning, optimization, and other powerful analytical models[8] with the potential to improve the value of hospital clinical care, but very few have been usefully implemented or scaled.[9,10]
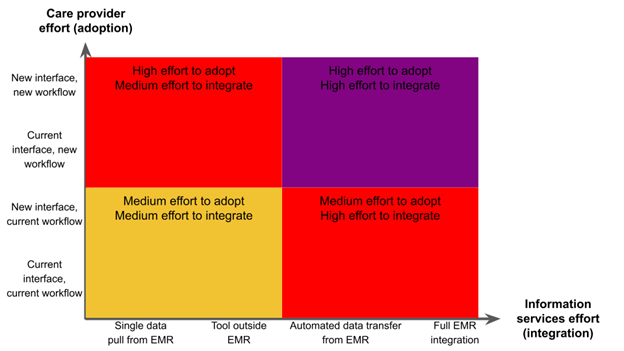
Low-productivity technologies are those that add elements to existing workflows and business processes, and serve to sustain existing business models.[11] In most cases, these innovations end up adding cost to the healthcare system, such as using CAT scans instead of routine X-rays. Reducing healthcare costs requires the adoption of high-productivity technology: technology that changes business processes, substitutes away from low-value care, reduces overhead and management costs, or disrupts existing business models. Most technology innovation in healthcare seems to be in the low-productivity category when we desperately need innovation in the high-productivity category. There is limited understanding of why the massive investments in health information technology have not been more successful. There are two dimensions to process improvements involving information technology: technology integration and care provider workflows (Figure 1). Most information technology innovation strategies focus first on the technology and then, if at all, on workflows. We examine efforts to implement process innovation across both dimensions.
Figure 1: Quadrants of institutional effort required for full implementation
The Technology-First Approach
The few EMR-integrated decision-support tools that have been adopted into provider workflows are exceptions that illustrate the rule. The most common approach is to train or develop models on historical data, integrate the model into the EMR, or deploy the model on a server that pulls data from the EMR, and then attempt to integrate the model into the workflow of the care providers. Several examples demonstrate the limited success, difficulty, or reliance on specialized tools, and expense of this approach.
Sepsis is a bacterial infection that can lead to organ failure and death if not recognized and treated early. It is a leading cause of death in hospitalized patients. Thus, early recognition of patients with sepsis has the potential for significant improvement in clinical outcomes. In theory, clinical data from an EMR can be used to identify sepsis, integrating laboratory data, medications, clinical condition, and patient vital sign information. Single-site studies have suggested the potential for adoption of machine learning algorithms using data from EMRs.[12] On the other hand, a proprietary sepsis prediction model tied to EPIC and implemented in hundreds of hospitals turned out to perform poorly when it was studied carefully.[13] It identified only 7% of those sepsis patients who were missed by clinicians. Meanwhile it generated sepsis alerts on 18% of patients, most of which were false alarms. It is common to see analytical models exhibit worse performance in practice than in development due to the reduced quality and quantity of data available during patient care. A different sepsis early warning system was successful[14], but its success was so unusual that an additional paper was written about its development and adoption.
A system for automated predictions of acute kidney injury depended on the infrastructure provided by the custom EMR used at the Department of Veterans Affairs and a specialized mobile medical assistant and alerting system.[15] Another healthcare system calculated the cost to validate and integrate a single algorithm for chronic kidney disease detection into clinical workflow was $217,138.[16]
Far more common, though less likely to be reported in prestigious journals or advertised by companies, are interventions that fail to make a difference such as a program to improve statin prescriptions.[17] These efforts are instead reported as a proof of concept.
Such efforts face two closely related barriers that prevent hospitals from effectively leveraging SaaS to redesign workflows with software integrated into their EMR. Care providers resist changes to their workflows, based on legitimate concerns about the uncertain performance of new technology. The larger the proposed change in workflow, the greater the odds that it will create unanticipated problems and the more effort is needed for development and testing (Vertical axis of Figure 1). Second, technical integration with the EMR is prohibitively time-consuming and expensive (Horizontal axis of Figure 1).[16]
Since hospital operations are based around EMR workflows, reducing reliance on EMR integration often necessitates reducing the extent to which new tools can reshape workflows. Numerous research groups and healthcare companies have turned to process redesigns that allow care providers to keep their current workflows and require only limited interaction with the EMR, such as a single initial data extract of historical EMR data stored in a data warehouse, a much lower bar than requiring EMR integration (Bottom left quadrant Figure 2).
The multibillion-dollar healthcare operations consulting industry often follows this strategy, typically performing historical analyses followed by suggestions for one-time processes redesigns. The value of the work of consultants depends on their skill, and there is little scale economy from one project to the next. This leads to slower improvements than from technology and software in other industries where a software developer can invest tens of millions of dollars to provide improvements to all users.
Technology companies serving hospitals have been forced to balance the efficiencies of improving software with the costs of providing consulting services. Technology startup LeaNTaaS was originally conceptualized as a SaaS company to improve productivity using EMR data, but the company was forced to pivot to a model with only a one time pull of historical EMR data to optimize the templates that schedulers use for infusion appointments.[18] The optimized templates are then manually entered into the EMR in a one-time update. The infusions clinic or hospital resumes its original workflows, and the templates facilitate more efficient scheduling. Similarly, QVentus, an early healthcare analytics SaaS company, transitioned to a software-empowered consulting model where its customers are “partners.”[19] A variety of academic groups have pursued one-time, data-driven updates to: surgical preference cards (supply lists) to reduce errors, and surgical blocks to improve access for emergency surgery or reduce variation in hospital census.[20–22] The simplicity of such approaches facilitates their implementation, but limits their potential to transform care delivery (Figure 2 diagonal).
An alternative approach to easing the barriers to implementation is to focus on tools that change only the software that care providers use, not their workflows or processes (Figure 1 tope left quadrant), or the tools that information services use (Figure 1 bottom right quadrant). This is the target of SaaS companies that focus on revenue management, data visualization or business intelligence, or staff scheduling. The Tableau data visualization software is increasingly popular with hospitals to save time generating and interacting with dashboards. Dashboards are suitable primarily for retrospective data review for managers, not for the implementation of more efficient, software-supported real-time workflows. Hospitals commonly use staff scheduling software that does not integrate with the EMR. Industry-leading scheduling tools such as Kronos require manual data entry, lack functionality compared to a tool that integrates with the EMR, and sometimes use paper timecards.[23] Such solutions have achieved significant scale across hospitals, but have limited relevance to more efficient, labor saving care delivery.
Figure 2: Tradeoffs between the effort required for implementation and the potential of the tool to transform care delivery
A Provider-First Approach
An alternative is to reverse the tech-first, workflow later approach. We propose meeting care providers and their workflows where they are by starting with the simplest possible version of the tool, or a one-time process redesign, and then iterating up along the workflow, EMR-integration diagonal. Such an approach reduces risk with an easier initial deployment and has the benefit of collecting data and feedback to improve in subsequent stages. It comes at the cost of a more labor-intensive and collaborative development process than e.g., building a ML model based on historical data in isolation from workflows or the constraints of the EMR.
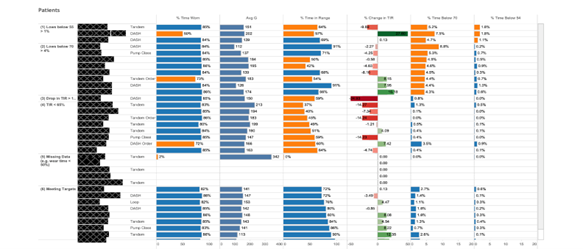
We recently reported on the design and deployment of an algorithm-enabled care model for personalized care at population scale.[24] TIDE (Timely Interventions for Diabetes Excellence) reduces provider screen time,[25] effectively analyzes data from continuous glucose monitors (CGMs) to identify patients in need of care provider attention, and is associated with improved type 1 diabetes management (lower HbA1C).[26] The key to the current success of TIDE is its iterative co-design by a team of care providers and engineers. TIDE started out as a simple, data visualization tool running locally on care provider laptops based on historical data manually pulled from the CGM manufacturer portal (Figure 3A).[25] It is currently an interactive dashboard that displays data generated by sophisticated algorithms, pulls data from the servers of the CGM manufacturer, and is hosted on a server with access to EPIC data (Figure 3B).
Figure 3: Initial and current versions of TIDE
3A Initial version of TIDE, no analytics, run locally on laptops, and requiring manual data downloads
Reproduced from [25] with the permission of the authors
3B Current version of TIDE, data pre-processed with sophisticated analytics, run on institution server, and automated data pulls
The initial, minor improvements in user workflows generated enough enthusiasm that providers participated in improving TIDE, and adapting their workflows based on those improvements. The data collected in the USE of TIDE were used to update TIDE’s algorithms and improve its specificity without any impact to workflows. Subsequent demonstrations of time savings for providers and improved clinical outcomes, generated enough institutional enthusiasm to dedicate the information resources to facilitate a more robust deployment of TIDE, and provided resources and priority to allow integration of TIDE with the EMR. At each step, the changes required, and the risk of failure, were significantly smaller than they would have been when asking an institution to adopt and integrate the final version of TIDE (Figure 4). The final version of TIDE is now available as an open-source tool for other institutions to use freely to manage their type-1 diabetes patient populations. It is designed for an initial launch of more limited, simpler functionality that expands along with the needs and the comfort level of the clinical team.
Figure 4: Transition from an an initial implementation of a modest tool that preserved workflows to a partially EMR-integrated tool that shapes workflows
Conclusions
These challenges of improving productivity with new technology are not unique to healthcare. Several decades ago, many industries faced similar problems with slow and awkward software development that resulted in expensive, inflexible and late system deliveries. This led to a collection of methods for rapid, less formal, user-centric, and incremental development under a number of labels such as “agile software development” and DevOps.[27] Reducing the effort required for software integration with the EMR will lower the barrier to technology adoption and lead to a pathway to high productivity innovation. Pressuring large EMRs to comply with the rules of the 21st Century Cures Act against data blocking would be a meaningful step in this direction.[28] It remains an open question how much IT companies that purchased EMR vendors will redesign EMRs to fit into the broader technical infrastructure of healthcare.
In the meantime, productivity efforts focused on care providers provide an opportunity for meaningful improvement. The agile, multi-stage, and co-development paradigms mitigate the risk of adoption failure without sacrificing the final impact of the use of the tool.
References
References
1. Papanicolas I, Woskie LR, Jha AK. Health Care Spending in the United States and Other High-Income Countries. JAMA. 2018;319(10):1024-1039. doi:10.1001/jama.2018.1150
2. Johnson S. Staff Shortages Choking U.S. Health Care System. US News & World Reports. Published online July 28, 2022. Accessed October 3, 2022. https://www.usnews.com/news/health-news/articles/2022-07-28/staff-shortages-choking-u-s-health-care-system
3. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516-529. doi:10.1111/joim.12752
4. Sahni NR, Huckman RS, Chigurupati A, Cutler DM. The IT Transformation Health Care Needs. Harvard Business Review. Published online November 1, 2017. Accessed October 2, 2022. https://hbr.org/2017/11/the-it-transformation-health-care-needs
5. Lindsay MR, Lytle K. Implementing Best Practices to Redesign Workflow and Optimize Nursing Documentation in the Electronic Health Record. Appl Clin Inform. 2022;13(3):711-719. doi:10.1055/a-1868-6431
6. Sutton DE, Fogel JR, Giard AS, Gulker LA, Ivory CH, Rosa AM. Defining an Essential Clinical Dataset for Admission Patient History to Reduce Nursing Documentation Burden. Appl Clin Inform. 2020;11(3):464-473. doi:10.1055/s-0040-1713634
7. The Nurse EHR Experience 2020 – Arch Report. Accessed October 2, 2022. https://klasresearch.com/archcollaborative/report/the-nurse-ehr-experience-2020/336
8. Mateen BA, Liley J, Denniston AK, Holmes CC, Vollmer SJ. Improving the quality of machine learning in health applications and clinical research. Nat Mach Intell. 2020;2(10):554-556. doi:10.1038/s42256-020-00239-1
9. Emanuel EJ, Wachter RM. Artificial Intelligence in Health Care: Will the Value Match the Hype? JAMA. 2019;321(23):2281-2282. doi:10.1001/jama.2019.4914
10. Simonite T. When It Comes to Health Care, AI Has a Long Way to Go. Wired. Accessed October 2, 2022. https://www.wired.com/story/health-care-ai-long-way-to-go/
11. Cahan EM, Kocher B, Bohn R. Why Isn’t Innovation Helping Reduce Health Care Costs? Health Affairs Forefront. doi:10.1377/forefront.20200602.168241
12. Sendak MP, Ratliff W, Sarro D, et al. Real-World Integration of a Sepsis Deep Learning Technology Into Routine Clinical Care: Implementation Study. JMIR Med Inform. 2020;8(7):e15182. doi:10.2196/15182
13. Wong A, Otles E, Donnelly JP, et al. External Validation of a Widely Implemented Proprietary Sepsis Prediction Model in Hospitalized Patients. JAMA Internal Medicine. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
14. Bates DW, Syrowatka A. Harnessing AI in sepsis care. Nat Med. 2022;28(7):1351-1352. doi:10.1038/s41591-022-01878-0
15. Tomašev N, Glorot X, Rae JW, et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature. 2019;572(7767):116-119. doi:10.1038/s41586-019-1390-1
16. Sendak MP, Balu S, Schulman KA. Barriers to Achieving Economies of Scale in Analysis of EHR Data. Appl Clin Inform. 2017;8(3):826-831. doi:10.4338/ACI-2017-03-CR-0046
17. Maddox TM. Clinical Decision Support in Statin Prescription—What We Can Learn From a Negative Outcome. JAMA Cardiology. 2021;6(1):48-49. doi:10.1001/jamacardio.2020.4756
18. iQueue Software for Infusion Centers – Healthcare Software. iQueue for Infusion Centers. Accessed October 3, 2022. https://leantaas.com/products/iqueue-for-infusion-centers/
19. Qventus Expert Services. Qventus, Inc. Accessed October 3, 2022. https://qventus.com/services/
20. Zenteno AC, Carnes T, Levi R, Daily BJ, Dunn PF. Systematic OR Block Allocation at a Large Academic Medical Center: Comprehensive Review on a Data-driven Surgical Scheduling Strategy. Annals of Surgery. 2016;264(6):973-981. doi:10.1097/SLA.0000000000001560
21. Zenteno AC, Carnes T, Levi R, et al. Pooled Open Blocks Shorten Wait Times for Nonelective Surgical Cases. Ann Surg. 2015;262(1):60-67. doi:10.1097/SLA.0000000000001003
22. Scheinker D, Hollingsworth M, Brody A, et al. The design and evaluation of a novel algorithm for automated preference card optimization. Journal of the American Medical Informatics Association. 2021;28(6):1088-1097. doi:10.1093/jamia/ocaa275
23. Kronos Alternative for Workforce Management. Smartlinx Solutions. Accessed October 3, 2022. https://www.smartlinx.com/kronos-alternative-workforce-management-software/
24. Scheinker D, Prahalad P, Johari R, Maahs DM, Majzun R. A New Technology-Enabled Care Model for Pediatric Type 1 Diabetes. NEJM Catalyst. 3(5):CAT.21.0438. doi:10.1056/CAT.21.0438
25. Scheinker D, Gu A, Grossman J, et al. Algorithm-Enabled, Personalized Glucose Management for Type 1 Diabetes at the Population Scale: Prospective Evaluation in Clinical Practice. JMIR Diabetes. 2022;7(2):e27284. doi:10.2196/27284
26. Prahalad P, Ding VY, Zaharieva DP, et al. Teamwork, Targets, Technology, and Tight Control in Newly Diagnosed Type 1 Diabetes: the Pilot 4T Study. J Clin Endocrinol Metab. 2022;107(4):998-1008. doi:10.1210/clinem/dgab859
27. DevOps. In: Wikipedia. ; 2022. Accessed October 3, 2022. https://en.wikipedia.org/w/index.php?title=DevOps&oldid=1111007463
28. Information Blocking. AHIMA. Accessed October 3, 2022. https://www.ahima.org/news-publications/trending-topics/information-blocking/