Kelly H. McFarlane, Stanford University School of Medicine; David Scheinker, Stanford University School of Engineering, Clinical Excellence Research Center, Stanford University School of Medicine; Barak D. Richman, Duke University School of Law and Clinical Excellence Research Center, Stanford University School of Medicine; Jacqueline J. Vallon, Stanford University School of Engineering; and Kevin A. Schulman, Clinical Excellence Research Center, Stanford University School of Medicine
Contact: kevin.schulman@stanford.edu
Abstract
What is the message? The Relative Value Unit (RVU) system was originally intended to improve the efficiency and transparency of physician billing and to decrease differential payments between primary care and specialty physicians. (1) Within 10 years, it was clear the system was not performing as originally intended. (2) It is possible to vastly simplify the Work Relative Value Unit (WRVU) billing system while maintaining the current physician compensation scheme, suggesting that the complexity of the Resource-Based Relative Value Scale (RBRVS) system is adding unnecessary complexity without creating value.
What is the evidence? The authors constructed a substantially simplified RVU system, with only nine possible values, and implemented a simple retrospective comparison to the current RVU system, which has over 1,400 possible values, using three years of submitted charges based on RVU and Current Procedural Terminology (CPT) codes.
Timeline: Submitted: April 7, 2023; accepted after review: May 8, 2023.
Cite as: Kelly McFarlane, David Scheinker, Barak Richman, Jacqueline Vallon, Kevin Schulman. 2023. Differences in Physician Compensation Associated with Simplifications to the CPT/WRVU System. Health Management, Policy and Innovation (www.HMPI.org), Volume 8, Issue 1.
Introduction
The Relative Value Unit (RVU) system is so ubiquitous in professional billing that it is hard to recall that Medicare’s implementation of the RBRVS system in 1992 was intended as an experiment. The prior billing system, based on “customary, prevailing and reasonable charges,” was described as “inflationary and complex…irrational, inequitable, and possibly leading to abuse.”(1) Policymakers launched the new Resource-Based Relative Value Scale (RBRVS) system to simplify the billing process, aiming to “provide a level economic playing field for physicians, one based on the resources they expend providing services.”(1) In short, the RVU system was intended to improve the efficiency and transparency of physician billing and to decrease the differential payment between primary care and specialty physicians.
Within 10 years, it was clear the system was not decreasing payment disparities between different practices. One study found that the overall RVU volume per beneficiary for physicians’ work grew by 50% but decreased 4.2% for evaluation and management services.(2,3)
Scholars have focused much less energy assessing whether the RVU system achieved its other goal, to simplify payments and reduce administrative costs for physicians. Despite the intent of the RBRVS system to reduce complexity in the billing process, administrative costs can be as high as 14.5% of revenue for primary care physicians and even higher in other settings. (4)
It is time to look at the RBRVS at 30 to ask several important questions about this approach to physician payment. First, does the complexity of the RBRVS system add value to the delivery system? Second, are there less complex approaches to physician billing that should be considered as part of an effort to reduce administrative costs in health care?
Methods
We implemented a simple retrospective comparison of the current RVU system with a substantially simplified one. Using three years of submitted charges based on Current Procedural Terminology (CPT) and RVU codes from the Department of Medicine at Stanford Healthcare from 2016-2018, we tested whether an alternative, simplified RVU system would have offered physicians similar compensation.
We calculated the sum of the total Work Relative Value Units (WRVUs) tallied by each individual provider and the total WRVUs of each department. These actual WRVU totals determine physician payment. We then constructed a simple rounding scheme as an alternative WRVU system (Table 1). The individual WRVU values were bucketed into ranges of WVRU values and all assigned one number within that range. From this “simplified” system with the rounded values, we calculated alternative WRVU totals for those same individual providers and departments.
Table 1: Simplification Scheme for WRVU Values
| WRVU Range | Count of Individual Charges | Rounded WRVU Value |
| <0.26 | 23,967 | 0.25 |
| 0.26-0.50 | 24,182 | 0.5 |
| 0.51-1.00 | 59,874 | 1.0 |
| 1.01-3.00 | 265,424 | 2.0 |
| 3.01-5.00 | 131,591 | 4.0 |
| 5.01-10.00 | 95,448 | 7.5 |
| 10.01-20.00 | 43,049 | 15 |
| 20.01-50.00 | 12,022 | 35 |
| 50.01-100.00 | 650 | 75 |
| Total Entries | 656,207 |
The actual WRVU totals were then compared to the simplified WRVU totals. Each individual provider’s actual WRVU total as well as their percentage of the total WRVUs for the Department were compared to their total and percentage under the simplified WRVU. The same process was completed at the Department level. A Wilcox paired t-test was performed to compare each actual value to the corresponding simplified value. The null hypothesis is that the true difference (location shift) between the actual WRVU totals for each provider and the totals under the simplified scheme is equal to zero.
Results
There are 656,207 individual submitted charges in the database. These charges correspond to 844 unique CPT codes and 1431 unique WRVU values. The charges were submitted on behalf of 737 different providers across 12 divisions within the Department of Medicine. The range of WRVU values is from 0.01 to 97.06, with 77.0% of recorded CPT codes corresponding to WRVU amounts less than 5.01.
We then constructed a “simplified” RVU coding system that consisted of 9 categories; each category was assigned to a single WRVU number ranging from 0.25 to 75.0 (Table 1).
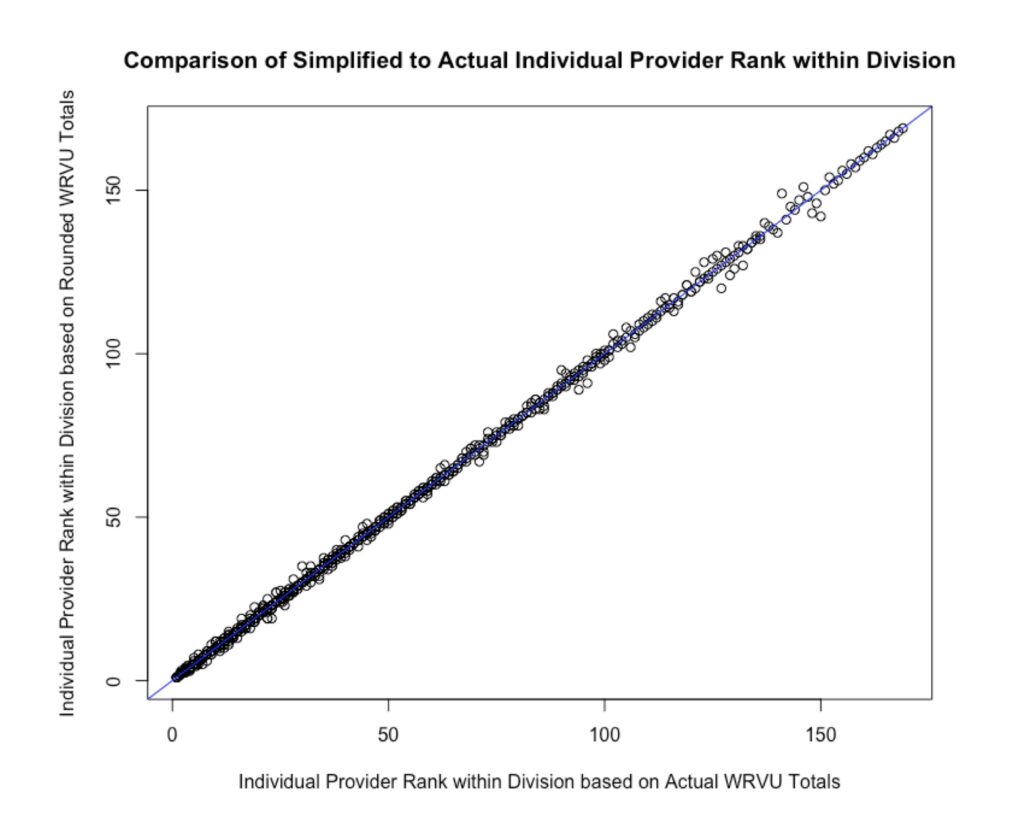
There were no statistically significant relative changes in compensation across providers, between the actual and simplified, with a wilcoxon p-value of 0.94, confirming our null hypothesis that the true difference (location shift) is equal to zero. Under the simplified system, 85.5% (618 of 723) of providers had ranks within their division that were either identical to their actual rankings or changed by only one position in either direction (Figure 1).
The results did not change significantly when the analysis was repeated for each year individually, with wilcoxon p-values of 0.91 for 2016, 0.73 for 2017, and 0.71 for 2018.
Discussion
After constructing a simplified WRVU system with only 9 categories and WRVU values, in contrast to the current system’s 844 categories and 1431 values, we found that our vastly simpler system would have led to nearly identical physician compensation – both in relative and absolute terms – as the current system did in 2016-18. As a proof-of-concept this suggests that providers could receive near-equivalent compensation under a much-simplified system.
This has important implications for the value of the RBRVS system in the billing process. In practice, RVUs are used to help incentivize and pay physicians based on the calculation of what fraction of the entire Department’s RVUs they contributed. If, however, the same outcomes can be achieved using many fewer categories, the additional complexity of the RBRVS system is unlikely to be adding value in the way it was intended.
The modern electronic medical records provide capability to implement more standardized, algorithmic care classification schemes. For example, a scheme with five categories (e.g., organ system, level of severity, level of complexity, medication category, and procedure category) with between 3 and 12 potential values for each category, would require only five inputs selectable from an auto-fillable field while allowing over 15,000 unique combinations. Such systems would allow significant flexibility and precision in documentation while offering a significantly simpler and more automated administration.
Our findings add urgency to debates that address unsustainable administrative costs in the US healthcare sector. The payment system is one of the most costly administrative tasks for hospitals. (4,5) A recent time-driven, activity-based costing study estimated the cost of billing and insurance systems contributed anywhere from $20 to $215 per encounter to healthcare costs.(4) Decreasing the complexity of billing codes would reduce the time and labor required in the billing process. Reducing optionality in billing and payment codes would also offer fewer opportunities to “upcode,” to employ coders and chart reviewers to extract additional revenue from either more billable items or more lucrative codes, and other costly and nefarious behaviors. (5) Since the government is the largest purchaser of US healthcare, policies to reform Medicare billing offer significant opportunities to simplify and integrate billing systems and reduce administrative costs. (5)
Though a certain level of clinical differentiation is still desirable, this can be accomplished without the complexity of today’s system. There are clearly other benefits to detailed billing systems, such as the generation of accurate data for research, but the requisite detail can be maintained with less complexity. Other approaches, such as utilizing a few categories in different combinations, could be utilized to provide additional variation while still simplifying the process from an administrative perspective.
The primary limitation of this study is that it was restricted to Department of Medicine codes and physician payments, and the simplification scheme was relatively simple. Given these results, even with a basic and vastly simplified rounding scheme, the opportunity to reduce complexity should be seriously considered.
Conclusion
Although the RBRVS system was initially intended to simplify the billing process, it appears that a far simpler system can work equally as well. It is possible to vastly simplify the WRVU billing system while maintaining the current physician compensation scheme, suggesting that the complexity of the RBRVS system is adding unnecessary complexity without creating value.
References
(1) Hsiao WC, Braun P, Dunn D, Becker ER, DeNicola M, Ketcham TR. Results and policy implications of the resource-based relative-value study. N Engl J Med; 1988 Sep 29;319(13):881-8.
(2) Chan DC, Huynh J, Studdert DM, Accuracy of Valuations of Surgical Procedures in the Medicare Fee Schedule. N Engl J Med 2019;380:1546-54.
(3) Maxwell S, Zuckerman S, Berenson RA. Use of Physicians’ Services under Medicare’s Resource-Based Payments. N Engl J Med 2007;356:1853-61.
(4) Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA. Administrative Costs Associated with Physician Billing and Insurance-Related Activities at an Academic Health Care System. JAMA. 2018;319(7):691-697.
(5) Kocher R. Reducing Administrative Waste in the US Health Care System. 2021;325(5):427-428. doi:10.1001/jama.2020.24767