Jianhong Wu is a University Distinguished Research Professor, a Canada Research Chair and an NSERC Industrial Research Chair, York University. His research expertise includes infectious disease modeling and data analytics to inform public health decision making and immunization program design and evaluation. He led national teams of disease modelling to support public health emergency rapid response for the SARS outbreak, the H1N1 influenza pandemic, and the COVID-19 pandemic.
Swift Mitigations and Tipping Point Cascade Effects: Rethinking COVID-19 Control and Prevention Measures to Prevent and Limit Future Outbreaks (York, Xi’an Jiaotong, Shaanxi Normal, 12/17)
Jianhong Wu, Biao Tang, Yanni Xiao, Sanyi Tang, Aria Ahmad, James Orbinski, York University, Xi’an Jiaotong University, and Shaanxi Normal University
Contact: orbinski@yorku.ca
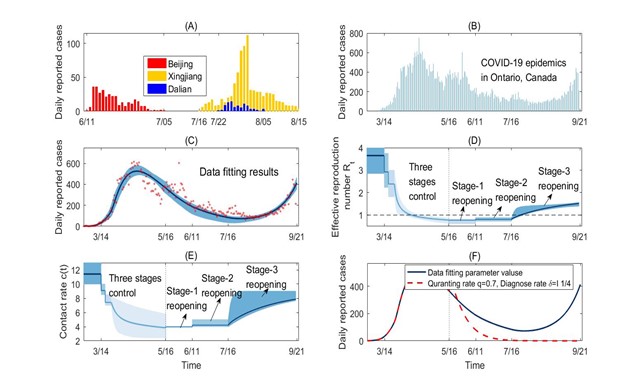
What is the message? Using data from the Canadian province of Ontario (March 12 to September 21, 2020), we model and identify the undesirable cascading effects of premature relaxation of social distancing. When the reproduction rate is near the 1.0 threshold, exponential growth from a large initial pool of SARS-Co-V-2 infections can quickly lead to outbreaks exceeding the contact tracing and testing capacities of public health systems. We then simulate the desirable cascading effects of mitigation interventions that are aimed at quickly reducing the reproduction number well below the 1.0 threshold. This enhancement can bring outbreaks to an end more quickly, and avoiding larger or full scale subsequent waves of transmission. What is the evidence? Using a mathematical model fitted to the Ontario data, we simulated a May 16, 2020 onset in Ontario of an increased quarantine proportion from 40% to 70% and a case detection period shortened from 7.5 to 4 days. With this enhanced testing and contact tracing capacity, the reproduction number would have dropped from 0.78 to 0.3 at the time of Stage 1 reopening. The accelerated rate of case decline across the Province would have ended the first outbreak by the end of June 2020, with a reopening that would have started with a significantly lower number of infections. Timeline: Submitted: December 13, 2020; accepted after revisions: December 16, 2020 Cite as: Jianhong Wu, Biao Tang, Yanni Xiao, Sanyi Tang, Aria Ahmad, James Orbinski. Swift Mitigations and Tipping Point Cascade Effects: Rethinking COVID-19 Control and Prevention Measures to Prevent and Limit Future Outbreaks. Health Management, Policy and Innovation (HMPI.org), volume 5, Issue 1, special issue on COVID-19, 2020.Abstract
All Countries are Attempting to Mitigate COVID-19, but with Varying Success
The ongoing COVID-19 pandemic has led to unprecedented mitigation policies designed to identify, contain, control, and prevent outbreaks of SARS-CoV-2 infection. Different jurisdictions have taken different approaches, with varying success. This article contrasts experience with mitigating the pandemic in China and in Ontario, Canada. We suggest strategies that can mitigate the pandemic more quickly and effectively.
Experience in China
Mainland China has achieved successful rapid responses to COVID-19 outbreaks, beginning with the complete lockdown of the first reported outbreak epicenter of Wuhan on January 23, 2020. By February 16, 2020, a month-long, nation-wide lockdown was expanded alongside the four-part “All Policy” – Quarantine All, Collect All, Detect All, Treat All.1 Collectively, these public health measures contributed to mainland China reporting no new cases by March 19, 2020. Following subsequent reopening, local outbreaks in Beijing, Xinjiang and Dalian were reported on June 11, July 7, and July 22, 2020 respectively. Swift lockdowns of provinces with affected cities coupled with expanded contact tracing, access to treatment, and rapid population-wide testing in areas with potential exposure to infection contributed to the success of no new cases in over a month, as shown in Figure 1(A).
When three cases of COVID-19 were confirmed on October 11, 2020 in Qingdao, the city was locked down. The governments’ pre-set scenario goal of immediate contact tracing and immediate testing of the entire Qingdao population (9 million) in five days was exceeded, as more than 10 million samples were collected and tested within four days. With 13 positive cases identified, the city was thereafter reopened. These “swift mitigation’” measures – rapidly reducing contacts followed by intensive contact tracing and widespread population testing —characterize the success of treatment, containment, and prevention in mainland China. From the peak to end of the first and -thus far- only wave of COVID-19 in the country, it took about 45 days. While this specific approach may not be feasible in all regions globally, the experience suggests key elements of a critical problem-solving strategy for subsequent waves of population transmission. Successful approaches need to invoke swift, focused and coherent mitigation interventions that are likely to be more effective than those that are piece-meal, poorly coordinated, and/or ill-timed.
Experience in Ontario, Canada
Modeling social distancing interventions: Initial reductions with risk of recurrence
A similar set of mitigation strategies was employed by governments around the world in their initial response to the first wave of SARS-CoV-2.2,3,4. Taking the Canadian province of Ontario as an example, we modelled a series of escalating social distancing mitigation interventions that were implemented in three consecutive stages between March 14 and May 16, 2020, followed by staggered de-escalation through to September 21, 2020 (Figure 1B). In addition to school closures (Stage 1) and restrictions to public events and recreational venues (Stage 2), the “swift mitigation” measures of shutting down all non-essential workplaces (Stage 3) was essential to reducing the Effective Reproduction Number, below the 1.0 threshold by on or around April 16, 2020.
This trend marked a strong start but was still susceptible to the emergency of new infections. Reflecting the sum effect of all mitigation interventions, when approaches the 1.0 threshold and the number of infections in the population is significant, a subsequent wave of infection is likely to emerge. A new wave is particularly likely where increased social contact allows for broader-based transmission, thereby driving above the 1.0 threshold.
Recurrence: April to September 2020
Using a transmission dynamics model fitted to the daily incidence data in Ontario (Figure 1C), we observed two key trends. First, although decreased to below 1.0 around April 16, 2020, it remained close to this threshold, resulting in only a slow case decline rate. Second, even with the quarantine proportion and case detection rate achieved at the end of Stage 3, can exceed the 1.0 threshold when the contact rate reaches only two-thirds of the normal full rate after reopening. This indeed happened when the province moved to regional de-escalation from Stage 3 on July 16, 2020 allowing businesses and public places in approved regions to re-open with safety and occupational measures in place.
Our estimation shows a gradual increase in the contact rate (Fig. 1E). However, contact tracing coverage and testing capacity remained relatively unchanged, with the quarantine proportion at 38% and a diagnostic testing confirmation period of 7.5 days after infection. As a result, the effective reproduction number gradually increased to 1.5, leading to a second wave in September 2020. In turn, the Province re-imposed modified Stage-2 mitigation measures in some hotspots.
Simulations: What if contact tracing had been higher and testing faster?
Using our model, we simulated a May 16, 2020 onset in Ontario of an increased quarantine proportion from 40% to 70% and a case detection period shortened from 7.5 to 4 days (Figure 1F). With this enhanced testing and contact tracing capacity, would have dropped from 0.78 to 0.30 at the time of Stage 1 reopening. The accelerated rate of case decline across the Province would have ended the first outbreak by the end of June 2020, with a reopening that would have started with a significantly lower number of undetected infections (if any). This would have allowed public health resources to be mobilized for swift and focused responses to any new localized hotspots, and likely avoiding a full-scale second wave of transmission.
In contrast to these desirable cascade effects – where enhanced social distancing measures maintain a low leading to reduced number of new infections, together with swift public health testing and contact tracing – Ontario experienced the undesirable cascade effects of pre-mature relaxation of social distancing. Unfortunately, as a result, the exponential growth from a large initial pool of undetected infections quickly led to outbreaks exceeding testing and tracing capacity. This negative cascade reinforced the resurgence of the pandemic in Ontario.
The power of tipping points: Triggers for a second wave in Ontario?
Stage 1 reopening in Ontario started on May 16, 2020 even as new cases continued to be reported daily, suggesting that may have been hovering around the 1.0 threshold. According to catastrophe theory and dynamic systems bifurcation theory, the province was at a “bifurcation point” with subsequent tipping point cascade effects, when de-escalation of social distancing began on May 16, 2020.
Tipping point cascade effects suggest that while a small increase to the bifurcation parameter (in this case, can trigger a second wave, further reduction of this bifurcation parameter near the tipping point can accelerate an exponential decline in new case transmissions. In Ontario, the number of total and new daily cases was judged to be “small” — wrongly, it appears — in deciding to begin reopening on May 16, 2020. Public health resources were likewise judged to be sufficient, instead of scaling testing, contact tracing, quarantine, and isolation efforts, which would lead to a further decrease of . Hence, the analysis suggests a missed opportunity to prevent the second wave.
Implications for Global Mitigation During the Second Wave
Similar situations globally can be identified on the WHO Coronavirus Disease Dashboard, with countries reporting subsequent waves of transmission with even larger peaks that have imposed significant challenges to public health systems in the face of public fatigue.5 Prolonged lockdowns have become a real possibility in many parts of the world. Yet this time, a critical problem-solving strategy for subsequent waves of COVID-19 population transmission should invoke swift, focused, and coherent mitigation interventions that aim to reduce the effective reproduction number well below the 1.0 threshold. This approach is likely to be more effective than strategies that are piece-meal, poorly coordinated, and ill-timed.
At least two factors have contributed to the occurrence of second waves in many countries. First, SARS-CoV-2 has high transmissibility with a high basic reproduction rate when activities resume.6,7 Second, although most countries implemented a range of public health mitigation interventions, implementation has often been lax and inconsistent, resulting in tipping point cascade effects that lead to further outbreaks.
One important strategy for controlling infectious disease outbreaks is to reduce below the 1.0 threshold. However, it is easy to stop too soon. Given the high transmissibility and reproduction rate of SARS-CoV-2, an effective reproduction number below but near this threshold could result in a prolonged period until the end of the outbreak.
Looking Forward
The global scale of the COVID-19 pandemic has catalyzed to significant advancements in public health interventions, including rapid testing and enhanced contact tracing capacities. With these, the period from peak to end of the second wave can and should be shortened when tipping point cascade effects are fully taken into account.
Effective strategies to confront subsequent waves of outbreaks and to safely reopen from full, staged or localized lockdowns require swift, focused, and coherent mitigation interventions to quickly reduce the effective reproduction number well below the 1.0 threshold. Enhancing public health mitigation efforts at the bifurcation tipping points can further accelerate the decline of new cases, followed by enhanced rapid testing and contact tracing when the case numbers are small.
Figure 1.
- Panel (A) Local outbreaks in Beijing, Xinjiang, and Dalian: shock mitigation and rapid testing enabled quick control8.
- Panel (B)-(F) COVID-19 epidemic in Ontario, Canada from Feb 26 to Sep 21, 2020. Here, the model by Biao et al.9 is used to evaluate the contact rates, diagnosis rate, and quarantine proportions, following the timelines of three stages of social distancing escalation to control the 1st wave, and the three stages of reopening. Social distancing de-escalation led Ontario to reopen on May 11. In our simulation (Fig 1F), with the quarantine proportion increased from 38% to 70% and diagnosis period shortened from 7.5 to 4 days starting on May 16, the reproduction number would have decreased with an accelerated rate of decline, such that the first outbreak would have ended by the end of June and the reopening would have started with very small number of infections. Public health resources could then have been mobilized for swift reaction to any new local hotspot to avoid a full scale second wave. In contrast to this desirable cascading effect — contact reduction leads to a small number of new infections and enables swift public health tracing and testing — Ontario experienced the undesirable cascading effects of relaxation of social distancing too early, such that the exponential growth from a large initial pool of infections quickly led to outbreaks exceeding the tracing and testing capacity.
Author detail: Jianhong Wu1,3,†, Biao Tang2,4,†, Yanni Xiao2,4, Sanyi Tang5, Aria Ahmad,6 James Orbinski6
1 Laboratory for Industrial and Applied Mathematics, Department of Mathematics and Statistics, York University, Toronto, Canada
2 Interdisciplinary Research Center for Mathematics and Life Sciences, Xi’an Jiaotong University, China
3 Fields-CQAM Laboratory of Mathematics for Public Health, York University, Toronto, Canada
4 School of Mathematics and Statistics, Xi’an Jiaotong University, Xi’an, China
5 School of Mathematics and Information Science, Shaanxi Normal University, Xi’an, China
6 Dahdaleh Institute for Global Health Research, York University, Toronto, Canada
† The two authors contributed equally
Author contributions: Conceptualization, J.W., B.T. and J.O.; validation and simulation, B.T.; data curation, B.T.; writing—original draft preparation, B.T., Y.X., and S.T.; writing—review and editing, J.W., B.T., and J.O.; All authors have read and agreed to the published version of the manuscript.
Funding: This research was funded by the Canadian Institute of Health Research (CIHR) 2019 Novel Coronavirus (COVID-19) rapid research program, the Canada Research Chair Program and the Natural Sciences and Engineering Research Council of Canada (JW), and the National Natural Science Foundation of China (grant numbers: 11631012 (YX, ST), 61772017, 12031010 (ST)).
Competing interests: The authors declare no competing interests.
References
- Xiao et al., Linking key intervention timing to rapid decline of the COVID-19 effective reproductive number to quantify lessons from mainland China, Int. J. Infect. Dis. 97, 296-298 (2020).
- S, Hsiang et al., The effect of large-scale anti-contagion policies on the COVID-19 pandemic, Nature, 584, 262–267 (2020).
- Tian et al., An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China, Science, 368, 638-642 (2020).
- J. Kucharski et al., Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study, Lancet Infect. Dis. 20(10), 1151-1160 (2020).
- WHO Coronavirus Disease (COVID-19) Dashboard, https://covid19.who.int/table. [Accessed at Oct 15, 2020].
- Sanche et al., High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg. Infect. Dis. 26(7), 1470-1477 (2020).
- Flaxman et al., Report 13: Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries.
- National Health Commission of the People’s Republic of China, http://www.nhc.gov.cn/xcs/yqfkdt/gzbd_index.shtml [Accessed on Oct. 26].
- Tang et al., De-escalation by reversing the escalation with a stronger synergistic package of contact tracing, quarantine, isolation and personal protection: Feasibility of preventing a covid-19 rebound in Ontario, Canada, as a case study. Biology 9(5), 100 (2020).
Health and Economic Trade-Offs of COVID Policies in Sub-Saharan Africa (Univ. of Michigan, Makerere Univ., 12/17)
Paul Clyde, University of Michigan, and Fred Matovu, Chrispus Mayora, and Peter Waiswa, Makerere University
Contact: pclyde@umich.edu
What is the Message? This article describes key changes in operations, communication, and security that are central to moving ahead effectively as we deal with COVID-19, including designation of specialty care facilities, creating emergency management plans, changing appointment policies, coordinating social distancing, managing hygiene protocols, and expanding testing. What is the Evidence? The authors draw upon their recent experience at relevant medical centers. Timeline: Submitted August 5, 2020; accepted after revisions: August 31, 2020 Cite as: Paul Clyde, Fred Matovu, Chrispus Mayora, Peter Waiswa. 2020. Children Are at Low Risk for COVID But at High Risk for the Policies Designed to Curb COVID. Health Management, Policy and Innovation (HMPI.org), Volume 5, Issue 1, special issue on COVID-19, December 2020Abstract
“Part of the challenge here is that we’ve lost the nuance. Some people are saying this is a hoax, it’s fake, it’s not serious. Other people may be saying it’s the worst thing in the world, a zombie apocalypse. It’s neither. This is a terrible pandemic. It has killed 130,000 Americans. It has sickened many, many more. And we don’t yet know what the long-term complications of some of the illness [are]. But it is true that 99% of people who get it will survive.”
— Former CDC Director Dr. Thomas Frieden. [i]
Attempts to curb the pandemic can affect other health and economic targets
Government actions taken in response to the pandemic are often credited or blamed for their effect on the disease itself; less so for the other, more indirect, costs of these actions such as reduced attention to other illnesses. Part of that may be the lack of concrete numbers. Decision makers naturally gravitate toward hard numbers, and hard numbers are most readily available for those who contract COVID and those who die with it. Mortality and morbidity that result from actions taken to try to prevent the spread of the disease are more difficult to measure, much less attribute to specific government policies.
Nonetheless, a number of organizations have started documenting these costs and developing estimates of their magnitude and severity. For example, with respect to non-COVID health consequences, clinicians are expecting an increase in cancer deaths due to delays in diagnosis and treatment in western markets[ii] or due to constraints occasioned by suspension of public transport in Africa.[iii] For similar reasons, heart disease,[iv] mental health and other chronic diseases can also be expected to increase.[v]
The economic consequences of government actions taken to curb the effects of COVID have been even less clear. Some point to the significant economic consequences even in Sweden, where the government has employed a relatively light touch, as evidence that the economic downturn is a result of consumer fear rather than government action. Others assert that, even if there are negative economic consequences from government actions, these surely pale in comparison to saving lives, implying that economic downturns don’t cost lives
Data that speak to the economic consequences of fear are relatively scarce just because we only have a few months to observe. Existing studies show that the lockdown itself, and not just fear, is having an effect though some suggest the lockdown accounts for a small portion of the economic downturn,[vi] while others suggest lockdowns account for most of the decline.[vii]
Looking at Sweden’s economy highlights another difficulty in isolating the effect of the lockdowns themselves. Preliminary estimates of Sweden’s GDP in the second quarter suggest that Sweden did not fare well even relative to its neighbors, as it saw GDP drop 8.6% in the second quarter of 2020. Sweden did, however, fare better than most European countries and than G7 countries except Japan,[viii] the only G7 country that also adopted a relatively light touch.[ix]
The problem with these comparisons is that, like the disease itself, the economic consequences of COVID responses are not confined to political boundaries. Producers rely on export markets and consumers and producers rely on imports. Thus, the citizens of Sweden and any other country will suffer the consequences of actions taken by governments all over the world, especially close trading partners.
The link between the economy and mortality rates is clearer, although the health consequences of an economic downturn manifest themselves in other ways as well. Just as COVID may have long term health effects short of death that are not well understood yet, an economic downturn affects other aspects of health and quality of life. Nonetheless, since mortality garners substantial attention with respect to COVID, we use research on the relationship between economic downturns and mortality to estimate the potential effect of the economic downturn associated with COVID on mortality alone. In an effort to be concrete and tractable, we focus on the mortality rate of a specific group: children under the age of five in Uganda.
Health and economic impact in sub-Saharan Africa
Since the COVID-19 virus started in Wuhan, China at the end of 2019, it has been both a surprise and a relief to see that the virus itself has killed relatively few people in sub-Sahara Africa. The economic effect has, however, been devastating.
In Uganda, the Ministry of Finance Planning and Economic Development released April 2020 trade statistics which revealed that exports had fallen by 34.3%. Imports declined by 38.5% over the same period. This decline is attributed partly to airport closures and travel restrictions more generally. As but one indication of the severe consequences implied by these figures, fully 42% of tax revenue for Uganda is collected through international trade.[x]
When households have enough income, they are able to make reasonable choices of nutritious foods and other essential goods and services for their household members but, when people do not have enough income, health suffers and mortality rates go up. Recent data from Uganda shows that outpatient visits, antenatal visits, live births in healthcare facilities, immunizations have all dropped and in many cases, dropped by more than 10% relative to the same period the year before. The number of children with low birth weight increased relative to the preceding year[xi]. Hence, the reduction in income has led to increased health risks. [xii]
We can quantify the effect of the COVID economic downturn on mortality by using previous estimates of the effect of sudden declines in GDP on mortality. The GDP growth rate in sub-Saharan Africa is expected to decrease by as much as 8%. A World Bank study predicted that GDP would decrease from 2.4% in 2019 to as low as -5.1% in 2020.[xiii] The IMF is expecting a decrease in GDP of 5.4% in 2020.[xiv] Given the pre-COVID expectations of a GDP increase, this implies a decrease of about 8%.
Using estimates from a study of the effect of the 2008 financial crisis on infant mortality, an 8% decrease in GDP per capita could result in almost 150,000 more infant deaths.[xv] Estimates from other studies on infants[xvi] and children under 5 are roughly consistent with this, suggesting an 8% decline in GDP could lead to hundreds of thousands more deaths of children under 5.[xvii]
Note that the decline in GDP estimated by the World Bank and IMF was for the overall economy. This will understate the effect on GDP per capita if population is growing, as it is, in sub-Sahara Africa. Thus, the impact of COVID on the economies in many countries in the region is such that hundreds of thousands of children could die. Indeed, that seems likely.
We need to pay attention to trade-offs
Decision makers in governments around the world are faced with difficult decisions. Already, more than one million people have contracted COVID and died. The true number may be higher if some have died with COVID even though the disease was not diagnosed or, instead, may be lower if some people had COVID but died due to some other disease.
The uncertainty surrounding that estimate is much less than the uncertainty about the number we have tried to estimate: the increase in deaths due to the economic consequences of COVID and actions taken to prevent it. It would be preferable to wait until the data on both COVID mortality and the economic effects were more reliable, but since decisions are being made in real time, we will have to make do with what we have in real time. It would be a serious mistake to dismiss either the costs or the benefits just because of the uncertainty.
Consider three points regarding the numbers we presented above.
First, we have looked only at the economic effect on the number of deaths of children under five in sub-Sahara Africa. We do not consider the effect of delayed diagnosis and treatment of other diseases either in Africa or other countries. We do not discuss the effect on the over-five year child population in sub-Sahara Africa and we do not discuss the effect of poverty in other countries. All of these populations will also be affected.
Second, government actions to stop COVID will not bring COVID related deaths to zero and are not solely responsible for the decrease in economic activity resulting from the pandemic. Even in the absence of government actions, there would be negative economic consequences from COVID. Many are fearful and would choose to stay home and engage in the economy less, even if governments allowed it. We discussed this earlier but have made no attempt to isolate the effect of government actions and separate them from the “natural” effects on the economy.
However, we have evidence that at least some of the economic consequences are a result of government policy – and some studies suggest policy is the cause of most of the economic downturn. Similarly, even when governments take relatively drastic actions they do not necessarily reduce mortality dramatically or permanently. The state of Michigan in the U.S., for instance, has a population that is very similar to Sweden’s, and its governor issued a shelter in place order for 2 months, closing many businesses, limiting the services offered by hospitals, and other limitations. Yet, despite the stricter measures, the number of deaths related to COVID are about 45% more in Michigan than in Sweden.
Third, the estimates for an increase in mortality rates in sub-Sahara Africa are extremely conservative because they are one-year estimates and many of the newly-impoverished individuals are likely to remain in poverty for many years to come. Thus, the number of deaths due to the economic downturn will be much higher than the estimates presented above. To give some idea of the long-term effect, we can return to the 2008 financial crisis. The World Bank estimated that 70 million people who would not otherwise have been in poverty would remain in poverty into 2020 as a result of the 2008 financial crisis.[xviii]
Looking forward
Globally, about 60 million people die in the world every year. At the current pace, more than 1.5 million will contract COVID and die. Oxfam posted a briefing stating that as many as 12,000 hunger deaths per day could be related to COVID.[xix] Remarkably, their “Actions Needed” did not mention anything about the deleterious effect on mortality of government actions designed to limit the effect of COVID.
But we know anecdotally that the actions governments take to limit COVID deaths have caused people to die.[xx] We know that hundreds of thousands of children under the age of 5 are likely to die as a result of the economic consequences of COVID. While fear may be driving some of the economic downturn, government policy is also affecting it and to the extent that it is, governments need to keep these consequences in mind the same way they consider the effect of the disease itself.
During this horrible pandemic our actions, whatever they are, have costs and consequences. It is therefore important that when developing government policies, we identify and evaluate these as best we can. Let us be done with saying that the tradeoff is between lives saved and the economy as if helping the economy does not also save lives.
Governments have an array of options available to them, and each contains its own set of costs and benefits. Requiring masks to be worn in public appears to pose few costs, while providing significant benefits by slowing the spread of the virus. By contrast, forcing businesses to stop offering services does pose a cost, and has economic consequences that extend beyond the borders of the governing authority. Stopping elective surgeries in areas that are not experiencing significant outbreaks is different from stopping elective surgeries in areas that are facing a shortage of hospital beds due to COVID. The decisions governments face right now are difficult, but let’s be clear: it is not a question of saving lives or not saving lives. Rather, it is a question of trying to protect the lives of people from one malady (COVID) as opposed to another (the consequences of serious economic decline and increased poverty). As Dr Frieden suggests in the quote at the beginning of this article, it requires a more nuanced approach.
References
[i] David Morgan CBS News July 6, 2020, and 12:33 Pm, “U.S. Is an ‘Outlier’ in Global Coronavirus Fight, Former CDC Director Says,” accessed September 21, 2020, https://www.cbsnews.com/news/coronavirus-united-states-former-cdc-director-tom-frieden/.
[ii] Norman E. Sharpless, “COVID-19 and Cancer,” Science 368, no. 6497 (June 19, 2020): 1290–1290, https://doi.org/10.1126/science.abd3377.
[iii] Geoffrey Mutegeki, “Covid 19: Delayed Treatment Puts Cancer Patients At Risk,” accessed September 21, 2020, https://www.newvision.co.ug/news/1517647/covid-19-delayed-treatment-cancer-patients-risk.
[iv] “Fear of COVID-19 Keeping More than Half of Heart Attack Patients Away from Hospitals,” accessed September 21, 2020, https://www.escardio.org/The-ESC/Press-Office/Press-releases/Fear-of-COVID-19-keeping-more-than-half-of-heart-attack-patients-away-from-hospitals, https://www.escardio.org/The-ESC/Press-Office/Press-releases/Fear-of-COVID-19-keeping-more-than-half-of-heart-attack-patients-away-from-hospitals.
[v] Steven H. Woolf et al., “Excess Deaths From COVID-19 and Other Causes, March-April 2020,” JAMA 324, no. 5 (August 4, 2020): 510–13, https://doi.org/10.1001/jama.2020.11787.
[vi] Austan Goolsbee and Chad Syverson, “Fear, Lockdown, and Diversion: Comparing Drivers of Pandemic Economic Decline 2020,” Working Paper, Working Paper Series (National Bureau of Economic Research, June 2020), https://doi.org/10.3386/w27432.
[vii] Olivier Coibion, Yuriy Gorodnichenko, and Michael Weber, “The Cost of the Covid-19 Crisis: Lockdowns, Macroeconomic Expectations, and Consumer Spending,” Working Paper, Working Paper Series (National Bureau of Economic Research, May 2020), https://doi.org/10.3386/w27141.
[viii] OECD, “GDP and Spending – Quarterly GDP – OECD Data,” OECD, accessed September 21, 2020, http://data.oecd.org/gdp/quarterly-gdp.htm.
[ix] Eric Feldman, “Did Japan’s Lenient Lockdown Conquer the Coronavirus? | The Regulatory Review,” June 10, 2020, https://www.theregreview.org/2020/06/10/feldman-japan-lenient-lockdown-conquer-coronavirus/.
[x] Ali Twaha, “Covid 19: Uganda’s Exports Decline By 34.3%,” accessed September 21, 2020, https://www.newvision.co.ug/news/1521359/covid-19-uganda-exports-decline-34.
[xi] Ministry of Health, Uganda, “Impact of COVID-19 Containment Measures on Reproductive Maternal Newborn Child Health and Adolescent Health and HIV Service Delivery and Utilization in Busoga Sub Region, Uganda,” August 2020.
[xii] Jed Friedman and Norbert Schady, “How Many Infants Likely Died in Africa as a Result of the 2008–2009 Global Financial Crisis?,” Health Economics 22, no. 5 (2013): 611–22, https://doi.org/10.1002/hec.2818.
[xiii] The World Bank, “Overview,” Text/HTML, World Bank, accessed September 21, 2020, https://www.worldbank.org/en/region/afr/overview.
[xiv] IMF, “Six Charts That Show Sub-Saharan Africa’s Sharpest Economic Contraction Since the 1970s,” IMF, accessed September 21, 2020, https://www.imf.org/en/News/Articles/2020/06/27/na062720-six-charts-show-how-the-economic-outlook-has-deteriorated-in-sub-saharan-africa-since-april.
[xv] Friedman and Schady, “How Many Infants Likely Died in Africa as a Result of the 2008–2009 Global Financial Crisis?”
[xvi] Sarah Baird, Jed Friedman, and Norbert Schady, “Aggregate Income Shocks and Infant Mortality in the Developing World,” The Review of Economics and Statistics 93, no. 3 (August 5, 2010): 847–56, https://doi.org/10.1162/REST_a_00084; Friedman and Schady, “How Many Infants Likely Died in Africa as a Result of the 2008–2009 Global Financial Crisis?”
[xvii] Stephan Klasen, “Poverty, Undernutrition, and Child Mortality: Some Inter-Regional Puzzles and Their Implications for Research and Policy,” The Journal of Economic Inequality 6, no. 1 (March 1, 2008): 89–115, https://doi.org/10.1007/s10888-007-9056-x.
[xviii] The World Bank, The World Bank Group’s Response to the Global Economic Crisis, Independent Evaluation Group Studies (The World Bank, 2011), https://doi.org/10.1596/978-0-8213-8665-1.
[xix] Oxfam, “The Hunger Virus: How COVID-19 Is Fueling Hunger In A Hungry World,” accessed September 21, 2020, /explore/research-publications/hunger-virus-how-covid-19-fueling-hunger-hungry-world/.
[xx] Evelyn Lirri, “How Uganda’s Tough Approach to Covid-19 Is Hurting Its Citizens,” accessed September 21, 2020, https://www.telegraph.co.uk/global-health/science-and-disease/ugandas-tough-approach-covid-19-hurting-citizens/.
The Role of Shared Services in Supporting Ontario’s Move to Bundled Care and Value-Based Procurement
Lauren M. Bell and Jiayan (Maggie) Chen, Innovation & Strategic Partnerships, Plexxus
Contact: maggie.chen@plexxus.ca
Abstract
What is the message? From the perspective of a shared services organization, the paper discusses some of the challenges in linking procurement to outcomes as a core component of bundled payments relative to the stage of maturity in implementing bundled care in Ontario, the largest province in Canada. Despite the challenges, value-based procurement for specific portions of the bundles is beginning to make a difference in the quality and cost of services in the province. Examples include procuring across the patient continuum to enable bundling implementation for hip and knee patients.
What is the evidence? The authors work with Plexxus, a leading Shared Services Organization in Ontario, which has pioneered value-based procurement for multiple hospitals in the province.
Timeline: Submitted September 11, 2020; accepted after review: September 17, 2020.
Cite as: Lauren Bell and Jiayan (Maggie) Chen. 2021. The Role of Shared Services in Supporting Ontario’s Move to Bundled Care – Understanding the Complexity of Aligning Procurement and Bundled Payments through Value-Based Procurement. Health Management, Policy and Innovation (HMPI.org), Volume 6, Issue 1, Winter 2021.
Bundled Care in Ontario – Background & Current State
Health systems worldwide have been adopting value-based healthcare models to deliver better patient outcomes at the same or lower costs. Ontario, Canada’s most populous province, has also been progressing towards a more value-based healthcare system through the gradual implementation of more integrated care delivery and funding models, commonly known as bundled care. Although bundled care is no longer an entirely new concept in the province, implementation has been incremental and spanning only several patient conditions.
Generally speaking, a fixed payment is allocated for a defined episode of care to a bundle holder who, in turn, works to arrange care for the patient across multiple care settings. This funding model aligns financial incentives with outcomes, promotes care coordination and integration, and improves patient satisfaction. The model also helps to reduce the cost of care by supporting and shifting care to less resource-intensive settings. In the literature, providing care through bundled payments has demonstrated promising results for improving the value of healthcare spending in Ontario and other jurisdictions, such as the U.S. and Netherlands. [1], [2]
Building on the foundation of Quality-Based Procedures (QBPs)[1] and the success of early pilot programs in Ontario, the Ministry of Health (MOH) began implementing bundled care programs at scale during the past couple of years. Since April 2019, a unilateral hip and knee bundle has been implemented across Ontario hospitals that perform joint replacement surgeries. For other bundles such as those that cover shoulder replacement surgeries, Ontario is taking a voluntary and phased approach to implementation due to the complexity of elements such as data collection, reporting, and wanting to assess lessons learned appropriately. [3]
Value-Based Procurement can Support Ontario’s Move to Bundled Care in Helping Purchasers Extract Greater Value from Suppliers and Align around Outcomes
The role of Plexxus
Recent analysis shows that Ontario spends close to 25% of its annual healthcare budget to procure products and services for healthcare providers to deliver patient care. [4] As one of the leading shared services organizations (SSOs) in the province, Plexxus, based in the Greater Toronto Area, focuses on delivering value through service excellence, collaboration, and scalable systems and processes to its 20 member and customer hospitals. Since its inception in 2006, Plexxus has achieved $350 million in savings through its fully integrated supply chain model, inclusive of a scalable digital platform (i.e., SAP) to enable efficient service delivery, advanced decision-making, and analytics.
In addition, Plexxus has significant expertise in complex procurements, with experience across a broad range of categories and competencies, including implementing the first provincial value-based procurement (VBP)[2]of implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy (CRTs) devices. Through applying the principles and practices of VBP, Plexxus has and continues to play a crucial role in successfully leading initiatives that create tangible improvements for hospitals and patients.
The opportunity for bundled care
Bundled care focuses on optimizing care provided across an entire patient pathway rather than individual components of the patient journey in isolation. The episode of care is defined by a best-practice care pathway spanning multiple care settings from hospitals to home and community service providers. By its nature, each pathway relies on both goods and services that SSOs such as Plexxus procure to support the effective delivery of patient care. However, the province’s current procurement model was established with a more sector-based view, where each sector has a very different approach to managing supply chain and procurement of goods and services. This presents a unique opportunity for the province to consider progressive approaches to procurement, such as opportunities to procure for a larger part of the patient pathway to further drive value for patients and purchasers.
Procurements for bundled episodes are a type of VBP that requires a myriad of products and services spanning multiple care settings. By factoring both quality and total cost of patient care into the procurement equation, the new VBP approach focuses on procuring products and services that bring the most value. Value can come in the form of procuring standardized products and services across the continuum of care, which helps narrow unnecessary variation in patient outcomes and drive additional efficiencies through product alignment. [4] For example, when patients move from one healthcare provider to another across a patient pathway, they should be treated with standardized supplies regardless of the care setting unless there is a substantial clinical reason to switch to a different product.
Value might also come from improving the quality of care and patient experience through collaborative purchasing decisions. When an acute care hospital procures medical devices for surgical patients, the hospital should work with their bundle partners, such as home care service providers, to source solutions that include both the devices and home monitoring technology. Compared to the traditional procurement approach driven by the lowest pricing for the surgical devices, the collaborative approach between the healthcare providers across the patient journey has shown to achieve improved patient outcomes and lowered costs for the health system. [4]
Value could also come from fulfilling value propositions for all stakeholders involved in the patient pathway or aligning the procurement to particular outcomes that should be achieved for patients. The provincial value-based procurement of ICDs is not aligned with a bundle but was instead related to procedure-based funding. However, the initiative has delivered value, not only for hospitals but also for patients, providers, and the broader health system by focusing on the importance of battery longevity for patients as an organizing principle. The lessons learned from the initiative, such as comprehensive physician engagement, listening to patients, and early market engagement, are efforts that can be leveraged to support procurement initiatives for bundled care.
The Benefits of Procuring for Outcomes is Clearly Outlined in the Literature; Why has Ontario Struggled to Mobilize this Type of Procurement at Scale?
There is much discussion about the benefits of moving towards procurement activities that consider the larger patient pathway and associated patient outcomes in the literature. However, the empirical evidence on whether procuring for bundled care has delivered on the targeted quality improvement and cost savings objectives remain scant and inconsistent. [5], [6] In this section, a list of challenges is identified with respect to mobilizing procurements to support bundled care from a SSO’s perspective.
Integrated funding policy is still sufficiently in its infancy to allow for the Ontario supply chain to fully address current procurement silos, such as procuring for the entire patient pathway.
Ontario has only touched the tip of the iceberg on implementing bundled payments, in part due to the complexity of payment models for new conditions. The ministry currently supports a diverse funding model that spans a global portion and patient-based funding elements, e.g., quality-based procedures for hospitals. Ontario’s many funding streams do not allow the hospitals to align all their purchasing efforts with the entire episode of care. The funding mechanism for QBPs was developed based on types and quantities of patients treated for a specific acute care procedure. This funding methodology does not contemplate care that might be required throughout the entire episode, such as home and community care. [7]
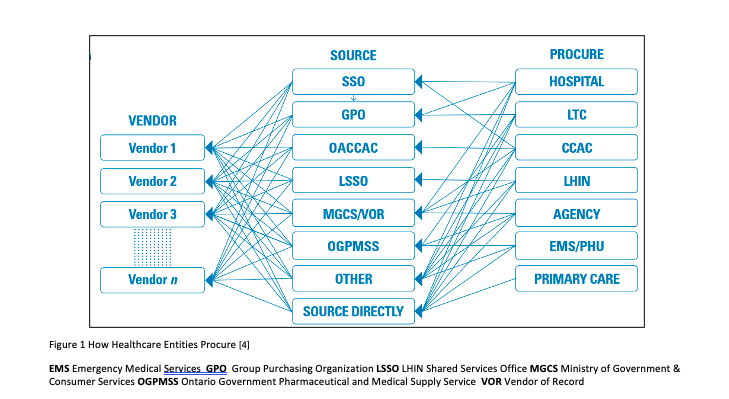
With this in mind, the current procurement model in Ontario has had to remain responsive to the dominant governance and funding structures, which result in highly fragmented and decentralized purchasing decisions. The fragmented decisions are furthered by each care setting — e.g., hospitals, LTC homes, home and community service providers — being supported by their own list of procurement entities.[3](See Figure 1)
Also, there is a diversity of business models within each procurement silo. For example, hospitals can technically procure through a GPO, SSO, government Vendor of Record, and/or their own internal hospital procurement departments. Moreover, procurement continues to operate in response to the dominant funding mechanisms that support more transactional purchasing activities based on annual funding cycles. The procurement approach limits the ability to meaningfully plan for go to market activities that consider a more comprehensive patient pathway and the total cost of care. The siloed funding and fragmented procurement environment have financially incented stakeholders to consider their best interest within a healthcare system that is constantly under financial pressure.
Similar to the mechanism of bundled care, the Ontario government could create an integrated funding policy to enable alignment of the different procurement silos and facilitate more opportunities to consider how to achieve greater financial efficiencies.
It is challenging to measure patient outcomes objectively and tie them to a specific intervention from a vendor. [6], [8]
The success of a VBP is not only measured on purchase price improvements but also defined by achieving value across dimensions that are identified upfront as core value opportunities. Compared to a traditional procurement that focuses on specific requirements and price, it is challenging to define, objectively measure, and fairly evaluate the “value” aspects of a value-based tender. It is even more challenging to reach a consensus on what value is among a wide array of government, health sector stakeholders, and vendors who participated in the VBP initiative.
The basis of a value-based tender evaluation is centered around patient outcomes. Through conversations with vendors, it is evident that they want to provide solutions to improve patient outcomes rather than just providing transactional products and services. However, patient outcomes are usually multi-factorial in a complex patient pathway, making it challenging to attribute any impact of outcomes to a specific vendor solution.
Also, most vendors, unless large consortiums are put in place, cannot be meaningfully embedded in the entire episode of care, making it difficult to deliver much beyond a portion of the patient pathway. Thus, it is often challenging to mobilize a single procurement for the entirety of a bundle, which holds vendors accountable for certain patient outcomes impacting the entire pathway.
When Plexxus engaged vendors on a value-based sourcing initiative, the SSO asked the vendors to propose solutions to improve their product usage on hospital-acquired infection rates. One vendor’s feedback was that any impact on the infection rate could not be directly linked to the performance of their or their competitors’ products. Multiple factors, including the selection of the products, can contribute to variations in the infection rate. Although the real-life example demonstrated the challenge of explicitly tying procurement to outcomes for an acute episode, it is reasonable to believe that procuring for the entire patient pathway could be even more challenging.
Purchasers often have minimal capacity to participate in procuring for the entire patient pathway. [6], [8]
Procurements to support the full bundled episode require a more complex type of value-based procurement. Thus, it requires more time, effort and a more focused contract management approach throughout the life of the agreement to ensure results are being realized. Early and consistent engagement with a substantial number of stakeholders such as healthcare providers, government, and other health system partners is imperative to ensure alignment on the goals and objectives that are being targeted.
More recently, purchasers such as hospitals have had limited clinical capacity to meaningfully invest in VBP relative to patient care and broader health system priorities that the hospitals must also support with already constrained resources. Since the start of the COVID-19 pandemic, Ontario hospitals are facing unprecedented capacity constraints to combat the pandemic. Among other competing demands such as resuming non-essential businesses and elective surgeries, preparing for a potential second surge, and assisting long-term care (LTC) homes, procurement initiatives to support bundled care are a lower priority for hospitals, resulting in many instances of direct negotiations and contracts.
In addition, the inability to procure for the entire patient pathway is not just a result of lacking hospital capacity but also the commitment to collaboration. Hospitals often cannot align for complex procurements due to various operating pressures and not being incented to act collaboratively. It is the hope this will begin to change as the province continues to support the implementation of the recent initiative of Ontario Health Teams.
Moreover, recent McKinsey physician surveys suggest that most respondents still do not have a solid understanding of value-based care or payment models. Thus, 21% of those physicians reported that they would be less likely to participate in those care models. [9] Furthermore, clinicians often want to maintain the status quo compared to exploring complex procurement approaches that can disrupt their usage preferences for specific products. As the role of VBP moves away from enabling clinical preference, increasing physician collaboration involves a significant amount of change management, communication, and strong system leadership from the government.
Examples of Early Wins Achieved from the Value-Based Procurement Initiatives Led by Plexxus
Hip and knee replacement bundles
Despite the challenges discussed in the previous section, several Plexxus hospitals have successfully leveraged procurement as a tool to generate greater value within the post-acute portion of the bundle, such as partnering with community service providers to design more integrated service models. In one instance, a procured home-care service model for hip and knee bundle patients helped ensure a seamless transition for those patients from hospital to home using allied health, nursing support, and virtual care while staying under the funded rate. The participating hospitals and the service provider arranged an up-front agreement on how benefits, both quantitative and qualitative, were measured and evaluated over time.
Key outcome measures for the hip and knee bundles, including readmission and length of stay, were established as the basis for ongoing review of project success. A risk and gain sharing model was also put in place to financially incentivize care collaboration and integration across the patient continuum, enabling bundled care implementation. The model allowed for shared savings between the hospital and the service provider where the direct impact was realized, and penalties if the cost per case exceeded the bundled pricing.
Provincial value-based procurement of implantable cardioverter defibrillators and cardiac resynchronization therapy devices
Even though the value-based procurement for ICDs and CRTs was tied to procedure-based funding, the initiative’s success is the empirical evidence of what a VBP could achieve for Ontario’s healthcare system. The Ministry of Health selected Plexxus to lead the first provincial value-based procurement initiative for ICDs and CRTs. Plexxus worked alongside physician leaders from Ontario’s 12 ICD Implanting Centers, partners, such as CorHealth Ontario and other SSOs, to develop a value-based procurement strategy to increase overall value for patients, and the broader healthcare system. Feedback received from patients such as device longevity, battery life, and MRI compatibility were included as critical considerations for the strategy to improve patient outcomes.
In order to incorporate device longevity into the procurement strategy, a robust longevity analysis methodology was developed to reward longer-lasting cardiac devices that improve patient experience. The approach used evidence-based inputs to support the evaluation of battery longevity. This is critical to moving procurement beyond a short-term decision to focus on the impact to patients over their lifetime. Fewer device replacements are directly related to better patient outcomes and reduced utilization of health system resources.
To support this undertaking, Plexxus established a provincial governance structure to support different elements of decision-making related to the core aspects of the procurement process as well as issues of broader policy and funding. The governance structure brought together clinical, administrative, and health system leadership, supported by a cross-functional team with representation from MOH, CorHealth Ontario, Plexxus, a health economist, and a fairness advisor.
Also, Plexxus developed a multi-phase evaluation approach for clinicians and administrators to meaningfully assess products and services that would address clinical requirements in addition to the hospitals’ business needs. To date, this initiative has demonstrated the benefits of a value-based procurement not only for participating hospitals but also for patients, providers, and the broader health system. It underscores the significant process considerations when designing non-traditional procurements. [10]
Looking Ahead
Ontario’s healthcare system is complex and highly-regulated. Continued efforts to create an environment that can align funding policy with procurement is an important enabler in the transition to a more value-based healthcare system. All healthcare stakeholders, including procurement organizations, aspire to maximize value for Ontario’s health system. However, disincentives and risks inherent from a single-payer system make it difficult for individual stakeholders to achieve better value single-handedly.
The implementation of bundled care will not fully succeed as a transformation activity if the province does not continue implementing integrated funding models at scale. A commitment from the province to scale up bundled care will fundamentally provide additional opportunities for procurement organizations to move away from traditional processes towards more replicable value-based procurement activities. With these building blocks in place, the vendor community can start to accommodate these new approaches by evolving their business models.
Furthermore, Ontario lags behind other jurisdictions when it comes to explicitly incorporating VBP into procurement policy. Ontario’s Broader Public Sector (BPS) Procurement Directive does not explicitly exclude value-based procurement practices. Nonetheless, it lacks clear guidelines to support the implementation of VBP. Through the ongoing evolution of our procurement framework, many stakeholders in the healthcare system could interpret the change in procurement policies as a signal from the government that procurement would eventually be seen as a more formal enabler to the achievement of high-quality care.
For example, the European Union (EU)’s new directive on public procurement encourages the implementation of value-based procurement approaches. [11] The directive also included “most economically advantageous tender” (MEAT) criteria as the procurement guideline for tender evaluation. Contrary to the traditional criteria that are predominately focused on pricing, the MEAT criteria take into account the price-quality ratio while also considering other longer-term costs related to socioeconomic impact and the environment. [11], [12]
In addition to a regulatory environment that supports VBP, a clear government mandate to encourage participation in value-based procurement initiatives is another critical enabler to fully realize the benefits. In the case of ICDs, while a formal mandate was not enacted, the ministry incentivized hospital participation by agreeing to hold funding flat for two years after the contract award. The mandate allows for any efficiencies to be reinvested in the relevant cardiac programs.
As per the structure of all SSOs, Plexxus currently has no direct relationship with the government except through the hospitals they support. As such, the ability to mobilize procurements and provide system leadership that can enable hospital and health sector innovation is often limited. While presently though there are no formal processes for SSOs to table value-based opportunities, Plexxus remains committed to being a strong business partner as Ontario continues its journey to become a more value-based healthcare system. This work will, draw on the organization’s broad supply chain management experience and expertise in value-based procurement.
References
[1] Hellsten E, Sutherland J. Integrated Funding: Connecting the Silos for the Healthcare We Need, C.D. Howe Institute, Commentary No. 463. 2017 January.
[2] Farrell M et al. Impact of Bundled Care in Ontario. International Journal of Integrated Care , 18(S2): A89, pp. 1-8, 2018.
[3] Ministry of Health. Bundled Care (Integrated Funding Models). 2018 April.
<http://www.health.gov.on.ca/en/pro/programs/ecfa/funding/ifm/>
[4] The Healthcare Sector Supply Chain Strategy Expert Panel. Advancing Healthcare in Ontario – Optimizing the Healthcare Supply Chain – A New Model. 2017 May.
[5] Steenhuis S et al. Unraveling the Complexity in the Design and Implementation of Bundled Payments: A Scoping Review of Key Elements from a Payer’s Perspective. The Milbank Quarterly. Vol. 98, No. 1, pp. 197-222.2020.
[6] Zelmer J. Canadian Foundation for Healthcare Improvement. Aligning Outcomes and Spending, Canadian Experiences with Value-based Healthcare.2018 August.
[7] Ministry of Health. Health System Funding Reform. 2015 September.
http://www.health.gov.on.ca/en/pro/programs/ecfa/funding/hs_funding.aspx
[8] Deloitte. How to eat the Value-based Procurement elephant? A Deloitte point of view.
2018 February.
[9] McKinsey & Company. Physician Employment: The Path forward in the COVID-19 era.
2020 July.
[10] Plexxus, Innovation & Strategic Partnerships. ICD Video Series on YouTube. 2019.
<https://www.youtube.com/watch?v=ypHa7Zjv5Pk&list=PL5EE1nUhb-0rAKgSSAGBzo7_aHrlKT4cM>
[11] Gerecke G et al. The Boston Consulting Group. Procurement – The Unexpected Driver of Value- Based HealthCare. 2015 December.
[12] World Economic Forum. Value in Healthcare – Laying the Foundation for Health System Transformation. In Collaboration with the Boston Consulting Group (BCG). 2017 April.
Notes:
[1] Both QBP and bundled care are new funding models introduced by MOH to link funding with quality. Bundled care is an evolved model, expanding on QBP funding methodology, which funds the entire patient pathway and aligns incentives with patient outcomes. QBP is a volume-based payment that aligns with funding for acute care procedures. Also, QBP clinical handbooks were developed by multi-disciplinary expert panels to include metrics, best practices, and evidence-based pathways for select patient populations. Some of the QBP clinical best practice recommendations were used to define the components of patient pathways for bundled care.
[2] VBP is a new procurement approach that incorporates the principles of value-based healthcare. Rather than focusing only on the lowest possible price, VBP focuses on procuring products and services that bring the greatest value to all stakeholders. The value is measured as the best outcomes at the lowest total costs over the full care cycle.
[3] Historically, local health integration networks and community care access centers also had unique procurement requirements, which now have been absorbed by Ontario Health.
The Long Fix: Solving America’s Healthcare Crisis with Strategies That Work for Everyone
Vivian S. Lee, Verily Life Sciences
Contact: vivianlee@verily.com
Abstract
What is the message?
U.S. healthcare needs multiple changes to be more effective: (1) pay for results, not action; (2) run healthcare delivery systems like businesses competing to deliver better health at lower costs; (3) demand that other health industries also compete on making people healthier at lower costs; and (4) learn from the successes of employer-driven and government-run health systems. Several successful ventures provide examples of how to do so.
What is the evidence?
The ideas are based on a recent book by the author, who has extensive experience in multiple U.S. healthcare systems.
Submitted: July 21, 2020; accepted after review August 6, 2020.
Cite as: Vivan Lee. 2021. The Long Fix: Solving America’s Health Care Crisis with Strategies That Work for Everyone. Health Management, Policy and Innovation (HMPI.org), Volume 6, Issue 1, Winter 2021.
The Miami Miracle
Chris Chen grinned as he remembered how people raved about his father’s clinic in Miami. His dad had scrambled to set up the clinic in the early 1990s. At the time, a few insurance companies were experimenting with new ways to pay doctors: giving them a fixed amount of money per patient, per year, no matter how sick a person was or became. If a patient needed expensive imaging studies, costly drugs or long hospitalizations that added up to more than that, it was the doctor’s problem.
Chris’s dad and mom—she was the office manager—opened their doors to patients in these new plans. They weren’t very busy, so they welcomed referrals. Other doctors sent them only their frailest and poorest patients, the ones they knew would be “grossly unprofitable” under this new way of paying. That’s how Chris’s parents began with 250 of the sickest people in Miami—people who would have been almost impossible to care for at any facility, at any price. It looked as if the Chens had signed up for a financial suicide mission.
Because resources were scarce and the patients needed so much, the Chens focused on primary care and prevention. These were fragile, elderly men and women who needed to be seen frequently by doctors—once they got sick, it would be too late—so monthly visits were set up, even if there was “nothing wrong.” Just getting to the clinic would be tough for many of them, so the Chens decided to provide free door-to-doctor transportation; they worked out that averting the cost of just one ambulance ride and hospital stay could pay for a year of shuttle service. A pharmacy was installed in the clinic so patients could conveniently, cheaply and reliably fill their prescriptions. And since elderly, frail, and poor people have an array of issues which make caring for them extremely complex, physicians in the clinics met several times each week to analyze how best to treat those who weren’t doing well.
Somehow, that “crazy Chinese doctor” and his wife not only gave outstanding care to all those seemingly hopeless cases—even those who couldn’t didn’t have enough money to pay their co-pays or deductibles—but they also managed to make them healthier. In fact, they reduced hospitalizations to one-third the expected rate. Even more amazing, they were able to break even financially. Simply, the Chens invented a better way to care for the elderly… and the rest of us.
The Fundamental Flaw
Healthcare is killing the economy, and in too many cases, killing us.
The system is bloated, wasteful and sometimes even dangerous. It is bad for patients, bad for doctors, and bad for business. For most Americans, the rising costs claim too much of their disposable income, and for most American companies, they are ravaging their bottom line. Beyond the outrageous cost of this care is its wildly varying quality. We all know from painful personal experiences that healthcare in this country delivers too few miracles and far too much stress, emotional and financial. It often seems as if no one is driving the bus, or that those at the wheel—doctors, hospital administrators, insurers, politicians—are swerving out of control.
Most of us trapped working in this system are desperately hoping for a better way. Many of us have successfully changed our practices to tackle important problems. For example, at Utah we created innovations like special catheter dressing kits that slashed the rate of blood infections in our burn care unit to zero. We also asked for patient feedback on all physicians, then posted all those comments online, and created a price transparency website so patients could estimate their out-of-pocket expenses.
Those changes and many others made us the safest teaching hospital in the country. In 2016, the University of Utah was ranked #1 in the nation among university hospitals for delivering the best care for our patients—the seventh straight year we made the Top 10.
Having interviewed hundreds of patients, clinicians, insurance executives, policy experts and journalists, I discovered real and practical solutions for how we all, working together, can build a safer, better, and cheaper healthcare system. Whether it’s frontline community health workers and patient families in Cincinnati, state employee health plan leaders in Washington state, palliative care doctors in Albuquerque, or the Chens of Miami and beyond, there are stellar examples all over this nation that prove it.
You may ask: If these leaders are improving the health of their communities, why aren’t their successes spreading more rapidly across the nation?
We Usually Pay For Action, Not Results
We all have to tackle the central and essential obstacle that is preventing real progress at a national scale.
This is the fundamental insight: The root cause of our maddening mess—inconsistent and unsafe care, unintelligible medical bills, inscrutable insurance plans, and inexplicable drug prices—is that insurers and government programs like Medicare and Medicaid pay for action, not results. They pay for every pill, MRI, lab test and operation, whether or not any of that makes us healthier. This arrangement has spurred massive growth in the industry and also generated an obscene amount of waste, from countless unnecessary operations and procedures to ever-more-expensive drugs that don’t work any better than generics. When people are compensated for doing something, independent of the results, they tend to do more and more of it. The primary motivation becomes getting paid, which may or may not get you healthy. That’s backwards and dangerous.
ChenMed Solution: Paid for Results, Delivering Results
For most doctors, it feels wrong to overtreat, to focus on profitability at the expense of health, and many of us are frustrated and even burned out. We want it to be different. Dr. Chen and his wife understood this. Their son, Chris Chen, who is now ChenMed’s CEO, has introduced this model of care into more than 50 primary care medical groups for seniors in Florida, Illinois, Louisiana, and Pennsylvania. At ChenMed clinics, instead of signing up as many patients as possible, which is the only way to support the fee-for-service (pay-for-action) model, physicians have fewer patients and spend more time with each of them.
Most primary care doctors in the U.S. handle over 2,000 patients; a ChenMed physician has between 450 and 600, which means they get to know the people in their care. Dr. Sofia Recabarren is a primary care physician who sees patients at a ChenMed clinic in Miami. She treasures the 40 minutes allotted for each new-patient visit and the 20 minutes for follow-up appointments, compared to half the time in her old job in New York City. “You actually know their meds,” she says. “You know what’s going on in their lives.”
That extra time matters. A lot. Chris Chen told me about a 400-lb. woman who, whenever she was asked what she had consumed for breakfast, lunch, and dinner, always gave answers which suggested she was eating sensibly. Chen was baffled over why she seemed unable to lose weight. One day, the woman’s daughter accompanied her mother for a follow-up visit. She thanked Chen for continuing to try to help her mom and then asked, “Can you get her to stop eating that bucket of KFC at midnight?”
Like all of the other physicians at ChenMed, Sofia Recabarren’s and Chris Chen’s goal is to keep their patients out of the hospital. One good way is to reduce the risk of falls and broken hips, instead of profiting from them. That’s why Dr. Recabarren has her patients take a short class to test how well they can see, checks their balance, makes sure their shoes fit well, and even gives tips for staying hydrated. She also encourages her patients to sign up for the clinic’s free Tai Chi course.
ChenMed clinics also understand that a person’s well-being is inextricably tied to overall health. They host monthly birthday bashes for patients—yes, their vans will bring you to this popular event and take you home after you’ve had your fill of cake, dancing, and gossip. These doctors know that loneliness is a killer. All over the world, physicians are starting to understand this and beginning to treat social isolation as a disease. In 2018, the British government appointed its first “minister for loneliness” to address isolation for citizens of all ages.
Other Examples
Physicians across the U.S. have adopted similar approaches to caring for patients in medical groups like Caremore, Leon Medical, Iora Health, and Oak Street Health, and ranging from California to Illinois to Massachusetts. They know it’s a better way to do medicine, and it’s also a better way to do business.
Studies show that ChenMed lowers the number of days patients are in the hospital by 38%. Same-day clinic visits mean that the number of expensive emergency department visits also drops. Chris Chen says clinics like his see at least a 25% increase in profitability. This model is so successful that Medicare has adopted it for its Medicare Advantage program. As an alternative to the regular Medicare program for seniors, Medicare Advantage is allowed to contract with doctors to pay them a fixed amount for keeping patients healthy. It is popular with seniors and projected to enroll over one-third of all Medicare patients in 2020.
The profound lesson learned by Chris Chen and his parents is that it’s far more effective to care for people before they get sick. And cheaper. That’s great news for those patients, but most of the U.S. is still paying an exorbitant penalty for ignoring that wisdom. Promoting health saves lives and money.
The Maddening Paradox: Best and Worst Health Care
By a few measures, the U.S. health care system is one of the best in the world and, by other measures, it is one of the worst.
The United States leads the world in medical innovation, and its scientists are discovering new cures at an exhilarating pace. The delivery of care, however is wildly uneven. Hands down, the United States spends more on healthcare per capita than any other nation— nearly one-fifth of the U.S. economy goes to pay for health. That’s two to three times more than other high income Organization for Economic Cooperation and Development (OECD) nations like the UK, Canada, Germany, Japan, and Australia, where health coverage is universal. Despite this about 1 in 11 Americans do not have health insurance and can’t afford care.
While most of the rest of the world is getting healthier and living longer, life expectancy in the United States is declining or, at best, flat. Babies born in the United States in 2017 are expected to live 78.6 years, 5.6 years less than those born in Japan, which places us 26th out of 35 OECD nations in life expectancy. The prospects for a healthier future are rapidly fading: Four out of ten adults are obese, and seven out of ten are overweight, making them much more likely to suffer from back and joint pain, and, over time, to be stricken by heart disease, stroke, type 2 diabetes, and certain types of cancer.
The nation is paying dearly for these failures. Companies that cover employee health insurance have seen rising costs that erode their margins and hobble competitiveness. Much of that ever-rising expense has been passed on to employees, often in hidden ways like flat wages over the past 50 years. Workers are also getting hurt directly, as deductibles and co-payments soar.
Healthcare is bankrupting the uninsured and the swelling ranks of the underinsured, and it’s often disappointing the millions who do have coverage. This ailing, failing system is making our nation sick— financially, emotionally, and physically. But within this seemingly barren healthcare crisis is not a spring but practically an ocean of opportunity.
Stop Paying More For Less
Reduce Expenses Not Care
With healthcare spending rapidly approaching $4 trillion per year, the obvious but misguided solution would be to reduce expenses by cutting care, but that’s dangerous for patients and for our future. It’s not care that needs to be cut, it’s the wasteful spending that doesn’t contribute to better health. We have to stop paying more to get less.
First and foremost, we need to reduce the waste. The Institute of Medicine (now National Academy of Medicine) estimated in 2012 that we waste 30 cents of every dollar we spend on health care. That’s over $1 trillion per year. Some of the waste is fraud and abuse, but most of it comes from failures to care for patients properly.
A substantial part of the waste is driven by overdiagnosis and overtreatment. In a 2016 survey, U.S. physicians concluded that about 20% of all medical care was unnecessary.
Additionally, ever driven to diagnose more ailments and perform more procedures, we are making deadly mistakes. Medical errors are the third-leading cause of death in the United States— over 250,000 deaths each year. That’s about 9.5% of all deaths, behind only heart disease and cancer. Many of the mistakes come from the inconsistent application of scientifically-derived guidelines. Physicians follow recommended guidelines only one- half to two- thirds of the time.
Besides the way we practice medicine, we are also choking on bureaucracy. In the United States, about 8% of spending on health care is spent on administration. Among ten high-income OECD nations, the figure averaged only 3%. Much of the bureaucracy burdens healthcare professionals who are paid generously but waste a lot of time. These expensive professionals waste a large percentage of their time on frustrating administrative tasks like computer data entry and disputing with insurance companies instead of caring for patients.
Because they generate the highest fees in a fee-for-service business, new technologies and treatments get advanced ahead of cheaper or generic alternatives. We spend double to triple what Canada and some European countries do on pharmaceuticals, mostly due to high-cost, branded drugs and the over-prescription of antibiotics and other medications. Prevention and primary care often are demoted in favor of specialty care.
Even at the end of life, we overtreat and overspend. We deny the wishes of the dying. We put people in hospitals who would be better off at home. In the hospital, we attach them to costly life support systems, even when they have asked to be left alone. While four out of five people would prefer to die at home, only one out of five does. Most people still die in a hospital or nursing home.
We are spending plenty, but not always in the right ways, and without getting what we want or what patients deserve.
Demanding Results not Action
Even those who are succeeding in the current fee-for-service model realize that paying for results— better health outcomes at lower costs— would radically improve our system. If our nation stopped expecting quick fixes— a prescription, a referral to a specialist, an MRI, an operation— and instead put a premium on measurably improving lives for good, then prevention would become paramount.
The medical world would focus on diet, sleep, and fitness. We would make restoring mental health as important as restoring physical health. We’d try to prescribe only drugs that work and that do so cost-effectively. We’d recommend imaging studies or operations shown to be beneficial. Back operations, for example, would be reserved for the few who truly needed them, and everyone else would be told to rest or undergo physical therapy. Hospitals and clinics would standardize care, making it safer and better. And those who didn’t would go out of business.
Who Cares? I Have Insurance
If the answer is so clear, then why isn’t the nation moving faster to paying for results?
For one, many have a vested interest in the status quo. Maybe even more important, most of us don’t really buy healthcare, we buy health insurance.
That means we don’t pay for healthcare directly, we pay for it indirectly, and even that is often subsidized. For about half of Americans, employers pay for most of their healthcare. For others, healthcare is a government benefit paid for by taxes. Only the 8.5% of Americans who remain uninsured pay for their healthcare bills directly—and mostly they can’t afford them.
With this insurance-based model, the dynamic between insurers and doctors can put them at odds with patients’ interests.
Consider a hypothetical small company, say, a book publishing house or a tech start-up with 200 employees. The president of the company engages an insurance company to provide health insurance to her employees. Each year that insurance company sets the annual premium rates based on predictions of how much healthcare her employees will need. The employer pays 70% to 80% of the premium; her employees contribute the remaining 20% to 30% through deductibles, co-payments, or coinsurance (see Notes for definitions). The insurance company then uses that pool of premiums to pay (reimburse) doctors, hospitals, pharmacies, and others for the care that employees and their families receive over the year. Instead of paying premiums to the insurer, larger employers who are self-insured will set the money in reserve to pay the health bills themselves.
In this arrangement, better health isn’t necessarily everyone’s goal: Insurers who pay doctors and hospitals for care are incentivized to spend as little as possible on a patient’s health. The less they pay out, the more profit they make. Conversely, in a pay-for-action model, most doctors and hospitals are incentivized to spend as much as possible.
This means patients—or more precisely, their premiums—are the rope in an annual trillion-dollar tug of war. Doctors and hospitals pull by ordering more tests and operations; insurers yank back by denying those services or adding restrictions like “prior authorization” paperwork for expensive medications and tests. When hospitals or doctors charge more than insurers are willing to pay, patients can get caught in the middle and be asked to pay the difference, leading to so-called “surprise bills.”
Usually, we expect competition in the market to drive innovation that leads to better services at lower costs. Not so here. Because we have an insurance model of paying for healthcare, the normal economic rules of the market don’t readily apply. For the insurance model to work, many healthy people have to enroll in a plan to offset the costs of unhealthy people. That’s a great deal for those who need expensive medications or a knee replacement, but a lousy one for those who don’t expect to use a lot of services. When healthy people opt out of such plans, leaving just the sicker and more expensive in the pool, premiums go up, and even the moderately healthy people are priced out.
This also means people who are insured have more incentive to get care they think they have already paid for, especially once they’ve spent their deductible. (“Use it or lose it!”) That drives costs up for everyone.
Leonard Saltz, a doctor at Memorial Sloan Kettering Cancer Center in New York City, explained it to me this way: “It’s like a dozen of us go out to dinner, and we’re going to split the check. You cleverly realize you might as well order the surf ’n’ turf instead of a cheeseburger, because you’re going to pay the same amount, regardless. That works until everybody orders lobster, and all of a sudden the check is much higher. That’s where we are in healthcare.”
When you take your child with a sore throat to the emergency room for a strep test that could be done in the clinic, undergo an MRI you probably don’t need, or fill unnecessary prescriptions — say, for an opioid pain medication or an antibiotic for a common cold — you or the doctor who prescribed it are piling on more and more “surf ’n’ turf.” And all of us are paying that grossly inflated dinner bill at the end of the night, which, in healthcare, means higher premiums for everyone next year.
What Are We Paying For?
Progress in fixing U.S. health has been held up by its daunting complexity, polarized politics, and many entrenched interests. Some argue for radical change— that the only solution is for the private insurance companies to be replaced by the federal government. Others believe in a totally free marketplace, including moving government-run programs like the Veterans Health Administration and military medicine to the private sector. Regardless of whether the payer is the government, an employer, or an insurance company, the root cause of our problem still needs addressing:
It’s not who runs the system that matters, it’s what they pay for that needs to change radically.
The Long Fix: A Revolution of Common Sense
The book that this article is drawn from tells the stories of some of the committed individuals on the frontlines who have experimented with new ways of practicing, built pilot programs, tested new technologies, and forged new partnerships to lay the groundwork for better care and a more workable system.
The Long Fix synthesizes and distills our collective ideas for this revolution of common sense into five main imperatives:
- Pay for results instead of action. The best investments in health engage people and keep them healthy, at home and independent and recognize the vital roles families and communities play (Chapters 1 and 2). Within hospitals and clinics, paying for health instead of paying for action creates the opportunity for health insurers and physicians to work together (instead of at odds with each other) to keep people healthier (Chapter 3).
- Run healthcare delivery systems like businesses competing to deliver better health at lower costs. Start with the highest priority of all: Make healthcare safer. Reduce medical mistakes by adapting better management models from other industries like manufacturing and aviation (Chapter 4). Improve the quality of care by making it easier to learn from experience, and tap into people’s intrinsic motivation to continuously improve (Chapter 5). Build tools that measure the costs of care as the first step to contain rising costs (Chapter 6). Treat patients like customers in the center of the healthcare universe and engage them as the most important coproducers of health (Chapter 7).
- Demand that other health industries also compete on making people healthier at lower costs. Pharmaceutical and device manufacturers should compete on the cost- effectiveness of their treatments. Entities like Medicare, which represents millions of patients, should be able to negotiate drug prices, armed with data about their effectiveness (Chapter 8). Patients’ electronic medical records should be used for the benefit of their health and to help doctors and hospitals improve the delivery of care (Chapter 9).
- Learn from the successes of employer-driven (Chapter 10) and government-run health systems (Chapter 11). Invaluable lessons from both models help us imagine a better healthcare system for America.
- Implement an action plan for the Long Fix that builds on the vital roles that everyone needs to play (Chapter 12).
The journey to better health won’t happen with a quick fix. As my old mentor Dr. B used to say, it may take a little more time than we expect, but it’ll be worth the ride.
The Promises and Challenges of Value-Based Care and Bundled Reimbursements in Single-Payer Health Systems
Brian R. Golden and Rosemary Hannam, Sandra Rotman Centre for Health Sector Strategy, Rotman School of Management
Contact: Brian.Golden@Rotman.Utoronto.Ca
Abstract
What is the message? On the surface, single-payer health systems seem especially well-suited to implement value-based, bundled payment initiatives. Focusing on a failed attempt to create a bundled payment system for wound care in the Canadian province of Ontario, we describe features of single-payer systems that are supportive of such initiatives, while also discussing features of single-payer systems that put them at a disadvantage. We examine the necessary links between strategic goals (e.g., achieving greater value), structure, and systems; the lessons learned from an early unsuccessful value-based care effort; and more recent successes based on these learnings.
What is the evidence? The authors helped design the Integrated Client Care Project in Ontario during the early 2010s.
Submitted: September 15, 2020; accepted after review September 28, 2020.
Cite as: Brian R. Golden & Rosemary Hannam. 2021. The Promises and Challenges of Value Based Care and Bundled Reimbursements in Single-Payer Health Systems. Health Management, Policy and Innovation (HMPI.org), Volume 6, Issue 1, Winter 2021.
Value Based Care May Help Solve Health Systems Fragmentation
Health system managers, policy makers, and scholars have long bemoaned the siloed, or fragmented, nature of health systems across the globe — some, of course, more fragmented than others. Michael Porter and Elizabeth Teisberg [1] seized upon this weakness of health systems, arguing that many providers along the value chain take extremely parochial perspectives, optimizing for themselves and sub-optimizing at the system level. They argued that this is manifested in, among other things, attempts to pass risk to other players in the system, the inability to attribute both positive and negative performance to providers, redundancies in care resulting in bloated costs, and poorly coordinated care for patients who are often left to navigate obtuse pathways to care.
The Porter and Teisberg framework popularized the concepts of value and bundled care, along with bundled payments, and has since been expanded in more recent work [2 3]. Because this framework is now well known, we will simply articulate the core principles here:
- Organize into Integrated Practice Units (IPUs)
- Measure outcomes and costs for every patient
- Move to bundled payments for care cycles
- Integrate care across separate facilities
- Expand excellent services across geography
- Build an enabling information technology platform
The two authors of this article, based in the Canadian province of Ontario, began conversations with Michael Porter shortly after the Porter and Teisberg framework began to show influence in several health systems, mainly outside of the U.S. (e.g., Sweden, Finland, Taiwan, Germany).[1] We three saw an opportunity to apply the principles of Value-Based Care, including bundled payments, in the politically important, fiscally significant, and by most accounts clinically challenged domain of home care services — and specifically, in the care associated with wound treatment. In order to educate Ontario health system leaders about the principles of Value-Based Care (VBC), we invited Porter to visit with health system leaders, subsequently followed by meetings and workshops in Boston with the two authors, Porter and his colleagues, and several Ontario health system leaders including two Ministers of Health.
This article describes our early experiences attempting to implement value-based care, including bundled payments, in Ontario beginning in 2008. Many of us leading the initiative, including government officials and the two authors, believed that a single-payer system was a particularly appropriate setting to implement VBC. Unfortunately, we were wrong. This initiative, referred to as the Integrated Client Care Project (ICCP) was, in our view and of an evaluation team’s, largely a failure [4] judged against the goals of implementing the VBC principles articulated by Porter and colleagues. However, as an early VBC initiative it was highly instructive for Ontario and later other provinces in understanding the challenges of implementing VBC, and bundled payments, in single-payer health systems.
In the remainder of this article we describe the provincial health system in Ontario (similar to most Canadian provinces), the ICCP, the challenges faced in its implementation, lessons learned, and more recent advances informed by our early VBC initiative. Central to our argument is that while single-payer systems may, on the surface, seem particularly amenable to the implementation of VBC, they also pose unique and significant challenges. Our perspective on these challenges, and ways to address them, are framed around the early organization-design work of Galbraith [5], extended by Golden and Martin [6] to the design of health systems.
Ontario’s Health System And The Integrated Client Care Project
Ontario is Canada’s most populous province with approximately 13 million of the country’s 33 million residents in 2008, the year the ICCP was launched. As are all provinces, Ontario is subject to the Canada Health Act of 1984, which created the current version of Medicare. The Act designates the provinces as the single-payer for all medically necessary health services and includes the following provisions:
- No user-fees or extra-billing
- Universality: Available to all Canadians[2]
- Comprehensive: Covers all medically necessary services
- Accessible: No barriers to use
- Portable between provinces
- Publicly administered
Coming out of our meetings with top Ontario government officials (i.e., the two health ministers), Michael Porter, and his colleagues, there was a view that the single-payer nature of Ontario’s health system — whereby the government is able to influence all providers by virtue of the funder’s “power of the purse” —- would overcome many of the challenges experienced at that time implementing VBC principles in health systems lacking unitary governance, such as across the U.S. Consequently, the two authors worked with the Ministry of Health (hereafter the “Ministry”) to identify a care setting for the province’s first VBC initiative. As part of a three-way collaboration between our research team, the Ministry and industry providers, the decision was made to launch the ICCP in the home care sector.
The ICCP was targeted at home-based wound-care. As described in an independent review of the ICCP outcomes:
Although not always recognized as a pressing health care problem, wounds are a common, complex, and costly condition [1]. Approximately 1.5 million Ontarians will sustain a pressure ulcer, 111,000 will develop a diabetic foot ulcer, and between 80,000 and 130,000 will develop a venous leg ulcer [1]…. The estimated cost to care for a pressure ulcer in the community in 2006 was $27,000 CDN… Community-based care for people with wounds is often fragmented and inconsistent, leading to prolonged healing times and ineffective use of resources. [4]
Importantly, clinical researchers in wound-care are largely in agreement about clinical best practices to treat wounds at home [7]. Additionally, there is consensus that quality care requires effective coordination and communication of an interprofessional team of physicians, nurses and other health-care providers working together. This interdependency among providers aligns with Porter’s concept of an Integrated Practice Unit whereby an interprofessional collective works together and is mutually accountable for outcomes.
Further arguing for our focus on wound-care, prior Ministry work had determined that there were significant departures from clinical best practice across the province, inconsistencies in outcome measurement and reporting — although there was consensus on the most appropriate outcome measures — and related, significant variation to the costs of care. Specifically, Shannon had recently shown that “best practice” resulted in a 60 percent saving over current practices. [7]
Pre- Integrated Client Care Project
Prior to the launch of the ICCP, home care for patients with wounds (e.g., diabetic foot ulcers, the focus of the ICCP) was provided by a variety of independent, uncoordinated healthcare professionals and organizations. The typical care pre-ICCP care model for patients is presented in Figure 1. As illustrated, a patient requiring wound care could be referred to the Community Care Access Centre (CCAC) — a provincially funded home care coordinating agency — by the patient’s hospital, through self-referral, or by a primary care provider. The CCAC would then assign a case manager whose role it was to assess the client’s care needs, authorize service, coordinate care, and provide system navigation. Medical supplies for the wound (dressings) would be ordered for patients according to their specific needs. Importantly, equipment needed by the patient was not covered by CCAC funding and could only be purchased by the patient if they had private insurance or qualified for government support.
On the surface, this CCAC case manager coordination appears well-designed and built around the patient. Ministry reviews, however, showed this not to be the case. For example, the nursing agency would complete a nursing assessment and develop a nursing “care plan.” Separately, the occupational therapy provider would visit the patient, conduct their own assessment, and complete another care plan. Likewise, for the nutrition service provider. Approximately sixty percent of each assessment by each specialized care provider, employed by different organizations, was identical to the one before and after it, with the remainder specific to their discipline.
Numerous other design features of the wound care process were known to impede effective care:
- Nurse’s generalist training versus the necessary wound care expertise; home care nurses were assigned by the case managers according to a contractually negotiated rota, and not based on specialized wound care expertise
- Fee for service contractual arrangements with all providers with no quality or patient outcome adjustments; progress defined as the number of treatment interactions
- Service typically provided by caregivers employed by different organizations, and these different organizations and their employees had no mechanisms to share information; each provider had its own, proprietary health record
- Patients would rarely be assigned a single caregiver, so even within a provider organization (e.g., nursing agency) continuity of care and inter-nurse communication was challenging
- Service providers requested supplies through the CCAC. Since there were often multiple providers in the home, with no mechanism to coordinate among them, it was common to over-order or to be short on supplies. This often resulted in unnecessary and costly extra visits when supplies were not delivered as planned (e.g., a nurse visiting the home to change dressings which had not been delivered)
We find an airline metaphor to be most useful in describing the disfunction of the pre-ICCP experience. Imagine boarding a flight where the captain, first-officer, and second officer meet for the first time moments before your flight, are employed and were trained by different airlines, for different aircraft, and speak different languages. Imagine the same sort of coming together, for the first time, for the cabin crew, mechanics, air traffic controllers, caterers. How comfortable would any one of us be on such a flight, even recognizing that the different ad-hoc teams (e.g., the cabin crew) have the luxury of being in the same “room” at the same time, and of course have the incentive — equal to passengers — of a successful flight?
The situation we witnessed in the wound care system was far worse than the flight example above; no such opportunity for coordination or flight-crew/passenger alignment of interests existed in Ontario’s home-care setting. Poor coordination and low-quality care only impacted the patient and the costs to the system but had no negative consequences to any of the provider organizations.
Figure 1
Integrated Client Care Project
The ICCP was designed to address the weaknesses by implementing the VBC framework of Porter and colleagues. Specifically, we designed a new approach of providing wound-care at home around six principles:
- Specialized case-management
- Coordinated assessment among providers
- System-wide navigation and integration
- Care delivered by integrated clinical service teams
- Informed by clinical best practice
- Rewards based on outcomes and encouraging innovation
The project was governed by a tri-partite structure made up of the Ministry, The Ontario Association of CCACs (OACCAC) and researchers at the University of Toronto. Importantly, ultimate decision-making authority lay with the Ministry.
The planned new model of care is reflected in Figure 2 and was undertaken in four of Ontario’s health regions. Under the ICCP, four[3] CCAC & home care agency pairs (one in each region) were selected through a voluntary application process to participate. The home care agency would be designated as the “bundler”. To illustrate, we refer to one of these bundler agencies as Home Care Ontario (HCO). HCO would be contacted by a CCAC case manager each time a patient met the criteria under the ICCP (e.g., suffering from a diabetic foot ulcer, at home, requiring inter-disciplinary team-based care).
Figure 2
Upon receiving notification from the CCAC after an initial assessment of needs, HCO would assign a clinical coordinator responsible for the collective activities — and outcomes —- of care providers. HCO’s coordinator, having prepared for a significant volume of similar clinical cases in the health region, would assemble a team of clinicians (e.g., nursing, nutritionists, occupational health, etc..) who specialize in the treatment of diabetic foot ulcers. As in the pre-ICCP era, some of these caregivers would be employed by organizations contracted by HCO. In other cases, HCO would hire these caregivers and bring these capabilities in-house. Communication between these specialized team members and between the team and the client would be now streamlined, a function of common training and purpose-built information systems/EMRs, the costs of which would be justified by the contractually guaranteed volume of cases assigned to HCO.
As part of the ICCP, HCO would receive a bundled payment that would be set by the Ministry at some to-be-determined price between the cost of best practice and the median price it was currently paying across the province. Recall the 3x fold difference between the current cost of care in Ontario versus the lower cost for best-practice care [7] awarded to HCO for meeting pre-determined evidence based outcome indicators (e.g., size of wound, healing rate, infection or other complication, wound related pain intensity. Naturally, potential bidders such as HCO would only bid for contracts based on its belief that it could deliver quality care at a cost below the price the Ministry had set.
Providing both an opportunity and incentive to HCO, coordinators were given the discretion to rebalance the time assigned to various care givers within its inter-disciplinary team (e.g., physio over more expensive nursing). HCO was also free to make evidence-based judgements around the use of supplies; supplies are closely connected to the effective care of wounds. For example, dressing A may require daily changes (which equals daily nursing visits) whereas dressing B may need changing only twice a week. Often, a dressing that requires fewer changes is more expensive, but there can be savings in terms of reduced healing times and fewer nursing visits. If the HCO team collectively controls both the supplies and the nursing visits, and knows and communicates the specifics of the client’s situation, they can view all inputs as a total package and, since they are being rewarded for outcomes and cost reduction, make the decision that will lead to the best, least expensive outcomes for the patient.
In another instance, HCO might make the decision to purchase of a $150 orthotic or air cast to relieve the pressure on an ulcer when walking. Pre-ICCP such devices could not be purchased by the CCAC. Under the bundled care project HCO could purchase this device as needed, thus leading the patient to ambulate more quickly, speeding recovery, reducing needed nursing visits, and also reduce total costs of care. As can be clearly seen, these examples of the planned bundled care and reimbursement provide a stark contrast to home care prior to the launch of the ICCP.
What actually happened?
The ICCP was launched in a system that seemed particularly amenable to implementing the principles of VBC, including bundled reimbursements. As mentioned above, the single-payer quality of Ontario’s system was expected to give the Ministry of Health the “power of the purse” to align the various design features of the health system needed to implement VBC. Further arguing for this initiative, the medical condition of diabetic foot ulcers was well aligned with the principles of VBC (e.g., well accepted and understood clinical best practices and quality measures, the requirement for multi-professional care, and significant opportunities to reduce costs). Yet, despite these positive prior conditions there was significant divergence between the ICCP intervention as intended and as implemented [4].
Our analysis of the reasons for this divergence is instructive for future VBC initiatives, particularly in single-payer systems. The analysis draws on the organization and system design framework presented in Figure 3 [5 6]. The underlying logic of this framework is that system structure, people systems, rewards, and information systems and decision support must be designed to support strategic goals, that all of these “points on the star” must be aligned — or supporting the others, and the decisions made about these points on the star (e.g., what to pay for and what not to pay for) influence the culture (i.e., values) of the organization/system.
We argue below that the ICCP was mainly unsuccessful due to the misalignment of these system design elements and that this misalignment was largely due to the cooptation of the project by the OACCAC. However, the ICCP was successful in germinating insights that have subsequently led to more successful value based and bundled payment initiatives.
Figure 3
The ICCP and the Star Model
Strategic Goals: The strategic goal of the ICCP was to provide better value for the payer and the patient. Specifically, this meant lower total costs, less variability in costs, and a better patient experience, including but not limited to clinical outcomes.
Structure: As illustrated in Figure 2, from a structural perspective, the ICCP was intended to bring all needed caregivers under one governance structure. Unfortunately, this never occurred. The Ministry, due to its long-standing conflicts with the Ontario Medical Association (essentially the physician’s trade union), was unwilling to broach the subject of structural and compensation changes with physicians. As a consequence, physician care —- central to the care and associated costs of wound care —- remained outside the IPU. Similarly, HCO as the “bundler” did not receive a contract for the full cycle of care for the wound as initially planned, nor any control over the pharmaceutical or the wound supplies budget, representing another limitation to how it could reallocate resources to achieve better value. Finally, the partner organizations that were part of the IPU and contracted by HCO were all separate corporations with no experience working with each other and unwilling to share proprietary costing data.
People Systems: By people systems we mean both kinds of people (e.g., nurses, physiotherapists) and how they are managed (e.g., training). Porter and his colleagues have argued that one of the benefits of IPUs is the opportunity to staff them with specialized caregivers. Unfortunately, the contract awarded to the “bundlers” (e.g., HCO) in the four regions did not provide sufficient patient volume to justify this kind of assignment or specialized training.
Other skill or experience deficiencies were also observed, and some were unique to single-payer government funded systems. For example, the bundlers and the providers they hoped to contract with lacked the governance skills of partnering and contracting. Also, Ontario’s health system has a dearth of professionals with actuarial skills; the historical payment models to providers did not account for patient characteristics.
As a result, both the Ministry and the bundlers lacked the skills to determine a reasonable level of bundled payments (Ministry) and the costs to provide care (HCO and its contracted partners). This led to a reluctance by the Ministry to set what it feared would be too high a bundled payment price and by HCO to seek a contract and bundled price from the Ministry as per the original plan, as they were unsure if the bundled price would cover their costs. The source of this lack of capabilities comes from the centrally planned, non-market environment of healthcare provision in Ontario.
Rewards: Central to the VBC framework is a payer which is able to determine a sufficiently attractive price, the bundled payment, to attract the interest of providers to form an IPU and make specialized investments that would result in improved outcomes for the dollars awarded providers. As described above, the critical physician services were carved out of the bundled payments. Also, because of a lack of historical market data, as well as actuarial and cost accounting capabilities, the Ministry was unable to determine a price somewhere in the “sweet spot” between what it was previously paying for foot ulcer care and the bundlers’ collective costs for providing care. In fact, the bundlers were not able to confidently determine their full costs of care, in part because of underdeveloped costing capabilities and because the organizations they planned to contract with were unwilling to share proprietary data. There was also a lack of confidence in defining eligibility criteria and including stop/loss provisions to cover unexpected exceptional cases. As a consequence, bundlers attempted, unsuccessfully, to negotiate a large safety cushion in their pricing to avoid possible cost overruns.
Information and Decision Support Systems: Porter and Lee [2] describe the critical role played by information systems vis-à-vis VBC. Again, partly because of the lack of market forces in the Ontario health system, but also because of historical funding practices (i.e., “global funding” such that providers would typically receive some inflation adjusted funding over the prior year, regardless of the volume or quality of care provided). The consequence of past practices, as well as the uncertainty of the ICCP’s future, bundlers were unwilling to invest in specialized information and decision systems. Those involved in the ICCP pilot projects had to track patient data manually, which ultimately proved to be overwhelming. As a consequence of this information deficiencies, providers such as HCO were reluctant to take on larger future contracts.
Lessons Learned and Applied
While single-payer, publicly funded systems should have an advantage over more fragmented systems in the implementation of VBC, and this appeared to be the case at the outset of ICCP, in fact many of the capabilities needed were underdeveloped or totally lacking. The ICCP exposed these unexpected deficiencies and as a result the four pilot sites for ICCP were unable to set up and align the four design elements (“points on the star”) needed to support the strategic goal of better outcomes for dollars spent. Nonetheless, and while disappointing at the time, this early failure had a positive effect in that the initial stages of exposing Ministry leadership to Porter and Teisberg’s ideas had seeded an appreciation for the benefits of VBC and a recognition that the alignment of strategy, structure, people, rewards and decision support systems would be critical to future successes.
In the remaining part of this paper we focus on subsequent VBC initiatives that benefited from the ICCP experiment and make recommendations for others going forward, particularly in single-payer systems. We have selected examples under each “point” on the star to illustrate recent progress.
Structure: The CEO of St. Joseph’s Healthcare System in Hamilton, Ontario was part of the group of industry leaders who travelled to Boston to attend Porter’s three-day VBC workshop, and upon return spent time exploring ways to introduce VBC in his health system. After two years of study, and supported by the Minister, St. Joseph’s introduced a VBC pilot project focused on five acute medical conditions – COPD, CHF, hip and knee joint replacements, and thoracic surgery.
The initiative, called the St. Joseph’s Integrated Comprehensive Care Program (SJ-ICCP), began in April 2012 and was more closely aligned to the principles of VBC, including bundled payments, than the home care ICCP. In particular, the Ministry would award St. Joseph’s a bundled payment for what had previously been discrete and fragmented payments to various providers.
There were two notable improvements over the prior failed ICCP. First, all care providers except for physicians were included in the bundle — and all of these providers were employed by one of St. Joseph’s owned corporate entities (e.g., hospitals, home care, long-term care, etc..). The “bundler” for home care services was not the CCAC but instead St. Joseph’s own home care agency, which meant it was possible to create and assign a consistent homecare team for patients once they were discharged from hospital. Supplies and equipment were also included. Second, although physicians were not included in the payment structure, they were included in the planning and implementation, and experienced many benefits of the VBC initiative including improved patient outcomes, shorter length of stay, increased physician productivity (and therefore higher fee-for-service income) and a vastly improved patient experience.[4]
People Systems: The SJ-ICCP in Hamilton also demonstrated the value of an expert team dedicated to caring for patients within each medical condition. Assigning specialized care providers, including coordinators and personal support workers (PSWs) who had specialized training, allowed the teams to provide patient-centered care of higher quality and lower costs. For example, common post-surgical issues could be handled by phone or a visit by a nurse, without triggering a visit by the patient to the hospital. This resulted in a better patient experience and lower provider costs.
In addition, a province-wide initiative announced in April 2012, called “Quality-Based Procedures” (QBP) introduced activity-based costing to Ontario hospitals, prompting the development of costing and actuarial skills within hospital finance teams and the Ministry. Beginning with hip and knee replacements and expanding to other surgical and medical conditions over the last eight years, the QBP movement has created incentives for hospitals to develop capabilities to track costs and improve efficiency [8]. It has also encouraged specialized care teams, similar to the SJ-ICCP, as well as partnering with rehabilitation services and home and community care providers.
Rewards: The introduction of QBPs, which sets a price for each procedure, prompted a series of consultations between government, academics, and clinical advising teams to create best practice pathways and to determine corresponding costs to arrive at a mutually-agreed upon price for each procedure. Details can be found on the Health Quality Ontario (now Ontario Health) website.
Information and Decision Support: The focus on QBPs in Ontario has sparked investments in information and decision support capabilities, particularly in hospitals; recall, the home care ICCP revealed the importance of – and deficiencies in — these capabilities in the health system. Since then, consistently measuring how much it costs to deliver all aspects of care for a knee replacement surgery, for example, and comparing this total cost to the QBP rate, has been recognized as an essential strategic capability within the hospital sector. Similar capabilities are now emerging in the home and community care sectors.
Although the intention is there, both the measurement of outcomes and inclusion of outcomes in the contract for care delivery, particularly those focused on the patient experience, is still in development [9]. Movement has been slow, but encouraging signs are appearing, for instance in pan-Canadian organizations such as the Canadian Foundation for Health Improvement, the Canadian Institute for Health Information, and Canada Health Infoway, which are now investing in tools to enable all providers to measure outcomes [10].
Ontario Health Teams: In 2019, building on the progress of individual pilot projects, the Ministry introduced a new organizational form to deliver care throughout Ontario — Ontario Health Teams:
“… groups of health care providers and organizations that are clinically and fiscally accountable for delivering a full and coordinated continuum of care to a defined geographic population.”[5]
This new model, similar to the U.S.’s accountable care organizations, is designed to bring together the progress made in each element described above, and lays the groundwork for VBC, including bundled payments. But like the ICCP, it will be imperative for physician services to be included in the bundles.
Currently the Ontario Medical Association remains hesitant to alter physician funding, stymieing attempts by the Ministry to create outcome-based bundled payments. Some optimism is called for, however, as VBC models, including bundled payments, may create the opportunity for physician groups to benefit from health system cost savings.
Looking Forward
Our interest in working with Ontario’s Ministry of Health was in leveraging some of the ostensible advantages of a single-payer system to implement the VBC principles articulated by Porter and colleagues. While single-payer systems have obvious advantages such as the government’s power of the purse, and legislative authority to mandate quality targets, our experience with the ICCP and later VBC initiatives reveals that single-payer systems may also lack the sophisticated systems necessary for successful implementation. As suggested above, precisely because they are single-payer systems — an in the case of Ontario, with only not-for-profit, community-based hospitals — they often lack costing and pricing systems, effective information systems to coordinate care and measure performance, and critical human resource capabilities such as actuarial skills found in more competitive market-based systems.
We remain optimistic that single-payer systems can benefit from the principles of VBC, and the implementation of bundled payments. However, before this promise will be realized, several challenges of system alignment must be addressed, and the alignment model presented here can be instructive.
Several questions embedded in that model will need to be addressed in the affirmative. For instance:
- Are there organization and governance structures in place to form IPUs and support cooperation among provider partners?
- Do payers, providers and their staff have the requisite human resource/people skills to support VBC, including pricing and costing capabilities, and partnering skills?
- Are there sufficient rewards to induce risk sharing between payers and providers? Are there mechanisms to assign rewards to the providers creating value for patients and payers?
- Are information and decision support systems available to providers to support the delivery of high value patient care, and to payers so they can monitor and reward performance?
Our experience with ICCP and subsequent VBC initiatives in Ontario shows that single-payer systems do have many features that make them amendable to rewarding for value, and doing so in the form of bundled payments. However, such systems also have historical and unique challenges that must be overcome to achieve the promise of Value-Based Care that so many health systems today are pursuing.
References:
[1] Porter, Michael E, and Elizabeth O. Teisberg. 2006. Redefining Health Care. Boston:
Harvard Business School Press.
[2] Porter, Michael E., and Thomas H. Lee. 2013. “The Strategy That Will Fix Health Care.” Harvard Business Review 91 (10): 50-70.
[3] Porter, Michael E, and Robert S. Kaplan. 2016. “How to Pay for Health Care.” Harvard Business Review 94 (7/8): 88-102.
[4] Zwarenstein, M, K Dainty, and S Sharif. 2015. “www.ices.on.ca.” March. Accessed September 13, 2020. https://www.ices.on.ca/~/media/Files/ICCP/ICC-Wound-Care-Evaluation-Final-Report.ashx?la=en-CA.
[5] Galbraith, JR. 2001. Designing Organizations: An Executive Guide to Strategy, Structure, and Process. San Francisco: Jossey-Bass Publishing.
[6] Golden, Brian R, and Roger L Martin. 2004. “Aligning the Stars: Using Systems Thinking to (Re)Design Canadian Healthcare.” Healthcare Quarterly 7 (4): 34-42.
[7] Shannon, Ronald J. 2007. “A Cost-Utility Evaluation of Best Practice Implementation of Leg and Foot Ulcer Care in the Ontario Community.” Wound Care Canada S53-S56.
[8] Trenaman, L, and Jason M Sutherland. 2020. “Moving from Volume to Value with Hospital Funding Policies in Canada.” HealthcarePapers 19 (2): 24-35.
[9] Sutherland, Jason M. 2019. “Using Data to Move from Volume to Value.”
HealthcarePapers 18 (4): 4-8.
[10] Horne, F, and Rachael Manion. 2019. “A Made-in-Canada Approach to Value-Based Healthcare.” HealthcarePapers 18 (4): 10-19.
Notes:
[1] Interestingly, in our conversations with Porter, he indicated the slower progress in influencing the U.S. system because of its extreme fragmentation.
[2] A small percentage of residents are excluded from the Canada Health Act, including indigenous Canadians (who have separately funded system)
[3] The four pairs included four separate CCACs and three home care agencies, as one agency was the partner in two regions.
[4] https://www.stjoes.ca/hospital-services/integrated-comprehensive-care-icc-
[5] http://health.gov.on.ca/en/pro/programs/connectedcare/oht/#:~:text=Ontario%20Health%20Teams%20are%20groups,to%20a%20defined%20geographic%20population.
Health Care Access, People, and Policy in a COVID World: A Discussion with Healthcare Industry Leaders
Steven G. Ullmann and Richard Westlund, University of Miami Herbert Business School
Contact: sullmann@bus.miami.edu
Abstract
What is the message? The annual conference of the University of Miami Center for Health Management and Policy identified key issues concerning healthcare access during the COVID era, many of which will continue post pandemic.
What is the evidence? The insights draw on the knowledge of executives, policy makers, and scholars with a deep base of experience in U.S. healthcare.
Timeline: Submitted January 12, 2021; accepted after revision: January 13, 2021.
Cite as: Steven G. Ullmann and Richard Westlund. 2021. Health Care Access, People, and Policy in a COVID World: A Discussion with Health Care Industry Leaders. Health Management, Policy and Innovation (HMPI.org), Volume 6, Issue 1, Winter 2021.
Insights from the Ninth Annual Business of Health Care Conference at the University of Miami
The University of Miami Center for Health Management and Policy recently held its ninth annual Business of Health Care Conference. This year’s theme was “Health Care Access, People and Policy, COVID-19 and Beyond.” Participants focused on some of the most pressing issues of the year, including the financial impact of the pandemic on providers and patients, as well as the social determinants of health, disparities in access to care and the importance of public sector support.
One of the sessions at this year’s conference included a panel made up of Matt Eyles, president and CEO of America’s Health Insurance Plans; Joseph Fifer, president and CEO of the Health Care Financial Management Association; Hallee Fischer-Wright, M.D., president and CEO of the Medical Group Management Association; Ernest Grant, president of the American Nurses Association; Barbara L. McAneny, M.D., former president of the American Medical Association; and Richard Pollack, president and CEO of the American Hospital Association. As such, nearly all the major sectors of the healthcare industry were represented in the discussions. Given the diversity of industry representatives, it is noteworthy that there was significant agreement on the numerous areas of policy discussion.
Access and the social determinants of health
Among the areas focused on by the panel and its moderator, Pat Geraghty, president and CEO of Florida Blue and its parent company, Guidewell, was on the theme of access, and in turn, the interrelationship with the social determinants of health. Access reflected both geographic access and financial access. As Dr. Grant of the American Nurses Association indicated, “Nurses can help address the social determinants of health and alleviate the burdens of doctors and hospitals.” Dr. Grant went on to indicate that underserved communities have been particularly vulnerable to death and serious illness during the COVID-19 pandemic. In addition, many are essential workers living paycheck to paycheck who cannot afford insurance and might not see a doctor.
A number of other aspects of access were discussed, many associated with COVID. As per Pollack, hospitals are having significant funding issues, limiting their ability to provide safety net services. Further, their costs have increased significantly. Non-COVID revenue is down and there are significantly more uninsured patients due to job loss. From an insurance perspective, Geraghty noted there is a need for comprehensive planning at the national level – not just with respect to COVID, but with other aspects of healthcare provision as well.
Challenges to physician practices
The physician sector has also been impacted significantly by the pandemic. Dr. McAneny and Dr. Fischer-Wright noted that physician practices have been facing higher costs with fewer specialty patients seeking care due to COVID-19 fears. Smaller medical practices continue to have problems accessing personal protection equipment. Further, with their lower census, smaller practices are also experiencing difficulty in accessing capital resources, an issue not experienced to as great an extent by larger medical practices. Those difficulties are of particular concern to inner city and rural areas where communities are reliant on their local physicians. Add to this is the long-term impact of having more than 20 million Americans infected by COVID. Although hospitals provide the acute care associated with the coronavirus, it will be physician practices that will be providing longer term care for a growing number of patients exhibiting chronic conditions associated with COVID such as lung disease, heart disease, and blood clotting issues.
Looking forward
Transparency in prices and quality
As we go forward, what can we expect? There was again relative consensus. Fifer spoke about the continued movement toward consumer-focused healthcare with an eye toward value, and hospitals will have to be a part of this process. But for this to work, Eyles said that there must be transparency regarding prices and quality. Pollack noted that the relevant cost figure for consumers is the out-of-pocket price, not the rate negotiated between the hospital and the insurance company. The value proposition, i.e., value equal to quality divided by cost, also reflects the need to look at alternatives to in-hospital care, including home care. As Eyles said, “There is always a need for acute facilities and personal care, but a shift to in-home services would help meet the social needs that drive so much of our healthcare costs.”
Changing roles for hospitals
And so, what is the role of the hospital going forward? As Pollack indicated, the hospital will always be needed for emergencies and surgical procedures, but it may be much more important to access other types of healthcare from more convenient locations. As Dr. Fischer-Wright said, there must be a focus on prevention, keeping people healthy. The aspect of social determinants of health again becomes quite important and the panel shared reflections on multiple aspects of it.
As the panelists indicated, hospitals continue to have significant financial issues in small towns and rural areas. Dr. McAneny reflected on the implications of the loss of such facilities, including the loss of basic and emergency services in the community, as well as the economic impact as healthcare facilities are oftentimes the most significant local employer. It was suggested that perhaps these facilities should have tax-supported emergency rooms, much like fire-rescue and police departments are tax-supported. This could become even more important, as per Eyles, as millions have lost their employer-based health insurance coverage. The Emergency Medical Treatment & Labor Act (EMTALA) requires emergency departments to provide emergency care regardless of the patient’s ability to pay. But with the unemployed uninsured population growing by the millions given the COVID-induced economic plight, the financial impact on already stressed facilities is enormous as a result of bad debt and the provision of charity care.
Continued need for the Patient Protection and Affordable Care Act
As the session and discussion came to a close, other timely issues were discussed. Regarding the Patient Protection and Affordable Care Act, the panelists agreed unanimously that the law be retained and built upon. Further, given the sheer enormity of the task and the logistics, they agreed that it will be well into the latter part of 2021 before vaccine distribution will be widespread and be able to demonstrate its effectiveness from a public health perspective.
Next Conversation: April 16
We will reconvene this panel, a featured aspect of our yearly conference, on April 16. It will be interesting to see where we are at that point in time as the theme will be, “The Business of Health Care: Post Elections.”
China COVID-19 Fallout Effects: An Analysis of Emergency Response to Non-COVID Needs
Hoyt Gong and Cecilia Wang, The Wharton School, University of Pennsylvania
Contact: hoytgong@wharton.upenn.edu | yixiwang@wharton.upenn.edu
Abstract
Lead Sentence: China’s emergency response system at the initial outbreak of COVID-19 left unintended fallout effects on non-COVID-19 patients as medical resources were rationed early in the pandemic.
What is the message? China’s emergency response system at the initial outbreak of COVID-19 left unintended fallout effects on non-COVID-19 patients as medical resources were rationed early in the pandemic. The authors scope the fallout impact on affected patients via a quantitative case study on kidney dialysis, confirm similar challenges with perspectives from Wuhan healthcare providers, and corroborate healthcare access scarcity sentiments among a general Chinese population. While these issues have been addressed over time as the health system has adjusted, the authors provide structural, cultural, and systematic recommendations that highlight ways of solving the problems earlier when similar challenges arise in the future. Opportunities include early precision risk measuring interventions, widespread federal telemedicine adoption, strategic plans to allocate medical resources in times of infectious disease outbreaks, and stakeholder collaboration to enable natural mutual aid and prioritized national health.
What is the evidence? Interviews with physicians and nurses in Wuhan (N=7), WeChat and Weibo patient study survey data (N=162 across 24 provinces), and authors’ implications drawn from analysis of early COVID-19 articles in China. The evidence was collected from February to March 2020, and the results were analyzed during April to May 2020.
Timeline: Submitted November 2, 2020; accepted after revision: December 10, 2020.
Cite as: Hoyt Gong and Cecilia Wang. 2021. China COVID-19 Fallout Effects: An Analysis of Emergency Response to non-COVID needs. Health Management, Policy and Innovation (hmpi.org), Volume 6, Issue 1, Winter 2021.
Early in the Pandemic, China Faced Challenges in Responding to non-COVID Medical Needs
As Wuhan’s Hubei province went on lockdown in January 2020, early Chinese media coverage captured the frontline COVID-19 response that would shortly emerge as a global pandemic. With unprecedented pace of usage, medical resources ran scarce and emergency response measures were placed across hospitals nation-wide for rationing. Scarcity in PPE, healthcare personnel, and delivery capacity led to fallout effects in other health departments as concentrated attention was placed on the COVID-19 response. We define fallout effects as constraints impeding ill, non-COVID-19 patients from seeking proper care.
This article explores the impact of the pandemic’s fallout effects on China’s non-COVID-19 sick population early in the pandemic, taking varying healthcare stakeholder perspectives and evaluating gaps in China’s existing emergency response system in the early emergence of COVID-19. To address these challenge gaps, the authors offer suggestions for China’s federal emergency response to prepare and respond quickly to future disease outbreaks.
A Three-part Study
This study was conducted starting from January through March 2020 at the peak first onset of COVID-19 in China. The key stakeholders addressed in this study were Chinese healthcare providers (physicians and nurses), Chinese citizens across varying general health status, and Chinese kidney dialysis patients. The following sections illustrate each study data component with methodology and results of analysis. We discuss a dialysis case study, interviews with healthcare providers, and an online survey.
Dialysis Case Study
The fallout effects of COVID-19 gained visibility early in the pandemic with stories in Wuhan such as that of nurse Zhang Qin and her late father who passed away in late January. Qin’s father suffered from long-term uremia that requires dialysis at hospitals three times per week. However, immediately when Wuhan closed, the city’s hospitals stopped providing many medical services to prevent the risk of intra-hospital transmission, including the dialysis that Qin’s father required. After being denied transfers to two other hospitals, Qin’s father passed away at home days later due to the lack of dialysis treatment.
“I was busy saving others, but I can’t save you. I am sorry and I love you so much, Dad.” —Nurse Zhang Qin
Caught in the pandemic response, Nurse Qin was brought to the frontlines in a Wuhan hospital working 10+ hour days every day without time off and was unable to help her father. Medical resource allocation heavily led to fallout damage in chronic disease, particular in this case of dialysis.
Following many heartbreaking stories, the authors provided an estimate of the number of dialysis patients that could be affected by the reallocation of resources in the hospitals. From the Chinese Society of Nephrology, there are currently 100 million people in China suffering from chronic kidney disease (CKD), with 1 million of them having end-stage renal disease (ESRD)1. These one million patients would require regular dialysis to sustain their lives. It is estimated that only about half of these patients receive their dialysis regularly, due to lack of appropriate facilities and education in many areas. By multiplying 50% to the total number of ESRD patients, Chinese Society of Nephrology concluded that at least 500,000 patients in China undergo regular dialysis.
Since no provincial-level dialysis statistics were publicly available, the authors decided to estimate the number of dialysis patients in Hubei Province using its demographics data. Hubei Province is a densely populated region, accounting for 4% of the national population. Assuming an equal distribution of dialysis patients, there would be 500,000 * 4% = 20,000 patients receiving regular dialysis in Hubei Province. Taking a conservative approach, the authors assumed that half of the dialysis patients in Hubei Province were affected, which brought us to a total of 20,000 * 50% = 10,000 affected dialysis patients.
The dialysis patients were denied access to care for several reasons. First, some hospitals were designated to treat only COVID patients and extremely emergent patients. This means that they shut down operations for many departments, including the dialysis centers within the hospitals. Second, patients and their families were afraid to enter the hospitals because of the concerns about potential infections. This point is further substantiated by the survey data below. Additionally, since the transportation was shut down between Wuhan and many neighboring cities and towns, patients who needed to travel to a different community to receive their dialysis now lost their channel.
The estimate of 10,000 affected dialysis patients is conservative. The actual number of patients could be even higher. Furthermore, there remained many other types of chronic patients, such as patients with cancer, HIV-AIDS, or cardiovascular diseases. These patients were likely to be affected by the same reason—that the hospitals relocated their resources to concentrate on COVID, leaving behind the non-COVID patients. Together, the number of affected chronic non-COVID patients in Hubei Province was high, shedding light into the fallout effects of COVID-19 in the earlier stages of the outbreak.
Interviews with Healthcare Providers
The authors conducted seven primary interviews with frontline physicians and nurses in hospitals within Wuhan, Hubei. All healthcare providers asked to stay anonymous The interviews were conducted in Chinese and the scripts of the responses were translated into English later. There were some barriers to finding enough interviewees, since many healthcare providers were either too busy at the time or unwilling to share their opinions on this controversial matter.
There were five main questions asked to each of the interviewees with regard to hospital operations, resource allocations, and emergency preparations. Across the board, the responses were similar and key illustrative information is recorded below. Note that each letter represents a different respondent, and the letter is not indicative of any identity of the interviewee.
- How many patients were in your department on a regular day vs. during COVID period?
A: “175 patients on a usual day, but only 2-3 patients per day now.”
B: “There are 11 wards in our department and only 2 of them are open now. It will be only one ward opening as of tomorrow.”
- How much medical resources have been deployed to treat COVID patients?
C: “More than 90% of nurses in our department and about 50% of doctors from unrelated departments were called to the frontline hospitals.”
D: “All outpatient departments were closed and all resources were sent to the Fever Clinic, Department of Infectious Diseases, and ICU.”
- How can patients with chronic diseases get appropriate treatment during this period?
A: “There is a severe lack of prescription drugs and even I myself, still working at the hospital now, can’t get my antihypertensive drugs.”
B: “Many patients living outside of Wuhan will seek medical care in Wuhan. However, with the strict lockdown policy, none of them was able to do that these days.”
E: “The oncology department has been used to receive and treat COVID-19 patients now. There are an estimate of 1000 hospital beds there and all the cancer patients have to go home.”
F: “I know there are 18 patients left in the Gastroenterology department as of today. For most departments, there will be a max of around 10 patients and a min of 2 to 3 patients.”
- What preventative measures were in place to minimize the risk of COVID infection in the hospital?
D: “Every patient going into the hospital needs to be checked with body temperatures and travel histories. There is a strict division between the COVID-19 section and the rest of the hospital.”
G: “The best preventative measure is not having people being in the hospital. Since most parts of the hospital were closed now, few patients actually come. It requires too much time and effort to confirm if someone is 100% COVID-negative. If they did come to the hospital, it may be a danger to other patients and physicians.”
- Does the hospital still treat emergent situations?
B: “The emergency department is still open, although only half the regular staff still work there. However, we have many fewer cases on average in the past two months because people just stayed at home.”
E: “The emergency department is still open but we cannot operate on any patients now. I had someone reaching out to me saying he cut his finger at work, but I can’t operate on him in the hospital. We just don’t have any anesthetists now.”
G: “Patients who arrive at the Emergency department are in much worse condition on average. People don’t want to show up to hospitals during this particular time unless it’s life-threatening.”
To summarize, healthcare providers generally agreed that the normal hospital operations were greatly affected and most resources were dedicated to COVID patients. This shift had a substantial impact on the non-COVID patients, especially chronic patients who need to go to the hospitals on a regular basis. There seemed to be a lesser impact on the emergent patients, although limitations still existed for patients who require surgeries and more complicated procedures.
Online Survey Data
The authors created and distributed an anonymous digital survey2 to Chinese citizens via the online platforms WeiBo and WeChat as the main mediums for outreach. The data collection period lasted for one month (February 2020 – March 2020) and the 163 survey respondents represented 24 Chinese provinces. The full questionnaire is referenced in the appendix.
The key results of the survey fall into three categories of respondents’ experiences with (1) drug shortages, (2) chronic disease, and (3) acute illness.
- Drug Shortages
As an aggregate, 10% of respondents noted they experienced drug shortage challenges, defined as a lack of pharmaceutical medication due to access constraints imposed as a fallout effect of COVID-19 response. Of this group, more than half (56%) said they were not using the available government online drug platform3. Survey results show that this lack of use was largely attributed to an absence of awareness that such a federal pharmaceutical repository exists. On average, four out of five Chinese citizens experiencing drug shortage issues that did not utilize the People’s Republic of China (PRC) national program did so only due to a lack of information about the program’s existence.
- Chronic Disease
Respondents were asked about their health status with regards to having some form of chronic disease that requires regular medication or hospital treatment. 20% of respondents (27 people) reported having such a condition, but only 37% of this group (10 people) were able to still seek care from their standard provider. The rest were unable to access hospitals for their chronic disease. These respondents further reported the chronic issues they faced and how they coped with the lack of access in Figures 1 and 2 below.
Figure 1: Proportional mapping of respondents facing chronic disease
Figure 2: Proportional mapping of how chronic disease patients adapted to lack of access
- Acute Illness
The final survey questions asked respondents to evaluate if they suffered from an acute illness and their resulting experience seeking medical care. Notably, of the 23 respondents who self-reported an acute illness condition, only 6 of these individuals (24%) chose to seek care in a hospital setting. These patients who were still able to attend reported that their quality of healthcare delivered was almost as high as prior to COVID, with a median 4.25 of 5 compared to pre-COVID-19 quality of care.
Hence while we observe that most acute illness patients were unable to seek care due to fallout effects, a minority of manageable patient acute illness cases were accepted. China’s hospitals in early COVID-19 days focused on tight triaging measures, maintaining relatively standard quality of care at the cost of turning away a majority of other patients.
Of the remaining 76% of acute illness patients who were unable to access hospitals for treatment, the breakdown for their rationale is described in Figure 3 below. These patients each reported multiple challenges towards their inability to access care, falling into four categories (listed in order of complaint frequency): (a) fear of infection from hospitals admitting COVID-19 patients, (b) resorting to taking at-home and community-sourced Western and Eastern medications, (c) physical traffic restriction barriers preventing transportation to hospitals, and (d) physical hospital closures.
Figure 3: Rationale breakdown of acute illness respondents’ lack of medical access
Recommendations
Our early analyses demonstrate gaps that emerged in non-COVID-19 patient care across Chinese patients and providers during early stages of the pandemic. While these fallout effects have been mitigated with China’s COVID-19 recovery that has phased in at the time of this manuscript’s delivery in late 2020, the early challenges can serve as lessons learned for future disease outbreak response efforts by the PRC. We describe the key takeaways for application towards a future preparedness and emergency response in China based on the study components.
Structural Recommendations
Enable precise risk identification interventions through early federal sponsorship: An early federal response via financing existing health technologies alone will not adequately respond to pandemic effects on all healthcare departments. The emergence of precision health and patient risk stratification modalities (e.g., contact tracing, health data collection) supports the structural ability to target resource delivery for at-risk groups that may otherwise be overlooked in the midst of a pandemic response. By identifying at-risk and infected patients, the Chinese government is able to target precise healthcare delivery information to specific populations, such as the PRC’s pharmacy delivery program for chronic disease patients and city road closures for at-risk patients within a hospital’s catchment area. China’s status as a one party dominant governing system and widespread Citizen adoption of multipurpose super apps such as WeChat uniquely positions the PRC to enable rapid precision health interventions acting on patient risk data.
Build widespread telemedicine capabilities that encourage rapid standard of care adoption: Capacity building in the wake of contagious (historically R0 > 1.5) disease spread requires an emphasis on remote telemedicine services and contained treatment facilities. To encourage a more resilient Chinese health system, PRC can emphasize adoption of digital telemedicine services (e.g., virtual health platforms; PRC’s pharmacy delivery fulfillment program) across provinces to drive rapid systematic adoption of the new standard of care.
Cultural Recommendations
Encouraging community self-mobilization as a positive step of natural mutual aid: The emergence of online communities such as WeChat groups that provide medical advice and hands-free medications to its chat members highlight the natural mutual aid that emerges within the community. This self-mobilization of Chinese citizens created spaces in the informal sector in which community support gave benefit to their health outcomes. The PRC has the ability to amplify the successes of these informal communities by nationally acknowledging and advocating natural mutual aid as positive grassroots endeavors.
PRC collaboration with many representative hospital units in provisioning greater medical authority: While the cultural context of China rests on a backdrop as a one party republic with final decision-making authority, there remains an opportunity to shift further decision making autonomy onto medical authorities when facing a national epidemic. Particularly crucial in the early stages of an outbreak, government officials must recognize the expertise lent by medical personnel and defer authority in order to prioritize the national healthcare interest.
Systematic Recommendations
Strategic allocation of medical resources in times of infectious disease outbreaks: One important factor leading to the fallout effects on non-COVID patients is the lack of appropriate medical resources for them. During the initial stages of COVID outbreak, the federal and local government decided to shift the majority of the resources to prevent and treat COVID patients. While this seems to have been effective in containing the COVID spread, non-COVID patients often lacked access to care. The government should prepare strategic plans, learning from the mistakes of this time, that specify clear divisions of resources among emergent vs. regular healthcare operations in times of public health crisis.
Construction of specialized hospitals and more dialysis centers: Most hospitals in China are large, generalized hospitals. The lack of specialized hospitals and certified clinics made it difficult for patients to go to the hospitals during a pandemics period. Patients may be concerned about the risk of infection by going to the hospitals or the lack of doctors in such hospitals. The construction of specialized hospitals can reduce the risks of non-COVID patients going to the hospitals for other healthcare needs. For example, the establishment of more dialysis centers will likely prevent tragedies such as the one that happened to Zhang Qin’s father.
Limitations of the Study
The study has several limitations. First, the primary data collection could face biases and errors. There was no publicly available data on the fallout effects in China given the short amount of time between the outbreak and the research. Second, the authors were not able to speak with as many healthcare providers as hoped given the timeline of the research and the level of sensitivity of the topic. The lack of coverage from some important hospitals in Wuhan may have left out some important aspects of analysis. Third, the survey data may not be an accurate representation of the overall demographics. The sampling bias existed because it is likely that people who encountered relevant problems were more willing to participate in the study than those who did not. Furthermore, most of the survey respondents range from age 20-50 and came from middle income families. It is likely that demographics that experienced more severe fallout effects of COVID, especially within the lower-income population, were not featured by the online survey.
Looking Forward
Our analysis from the case studies on chronic patients, interviews with front line healthcare providers, and a timely online survey all indicated that China’s emergency response system at the initial outbreak of COVID-19 left unintended fallout effects on non-COVID-19 patients. The unbalanced resource allocation towards COVID had corollary effects. Patients lacked access to basic health care services merely because they were not COVID patients, which caused tragic consequences to many patients and their families both in the short and long term.
Fortunately, the PRC recognized the tragic fallout effects and their policy responses adapted to these challenges by late March and early April. With most hospitals reopening for non-COVID patients starting in April, the majority of the observed fallout effects gradually receded. From follow-up discussions with the healthcare providers and some survey respondents who initially participated in this research, the authors concluded that most hospital operations and standard protocols had been restored in the areas studied.
For scholars interested in similar research topics of observing the fallout effects of COVID in different regions, similar methods and channels can be adopted. One leading advantage of the method is the timeliness of analysis. Had the studies been done later in the year, the authors may not have caught as much real-time stories and sentiments toward the government’s initial policy. The ability to identify the problems quickly will facilitate better policy-making and international collaborations to minimize similar risks. It is the hope that this study will help China and the world reflect on the fallout consequences of COVID response and be more prepared for future public health crises.
Appendix 1—Chinese Society of Nephrology
Chinese Society of Nephrology: http://www.csnchina.org/cn/news.asp?id=39.html
Appendix 2—Digital Survey
The digital questionnaire sent out via WeChat and other social media:
Figure 4: Snapshot of the introduction and the first two questions
Appendix 3—Available Online Drug Platform
Starting on February 26th, 2020, the Hubei government has published some online drug platforms on which people can register for the drugs they need and have them delivered. In the meantime, 50 designated pharmacies in Wuhan reopened for patients to pick up prescription drugs, some of which included an online ordering and delivery services.
Announcement from Health Commission of Hubei Province regarding online drug delivery platform, published on Feb 27th, 2020 (website in Chinese):
http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/fkdt/202002/t20200227_2160653.shtml
WeDoctor—the first online drug delivery and consultation services sponsored and supported by the Chinese government following COVID outbreak: https://promo.guahao.com
Healthcare Post-COVID-19: Transitioning Healthcare Delivery Models to a “New-Normal” (Premier Cardiology, 9/10)
Vikrum Malhotra MD, Avni Thakore MD, Monika Minhas, Manpreet Kaur
Contact: vikrum.malhotra@gmail.com
What is the Message? This article describes key changes in operations, communication, and security that are central to moving ahead effectively as we deal with COVID-19, including designation of specialty care facilities, creating emergency management plans, changing appointment policies, coordinating social distancing, managing hygiene protocols, and expanding testing. What is the Evidence? The authors draw upon their recent experience at relevant medical centers. Timeline: Submitted August 5, 2020; accepted after revisions: August 31, 2020 Cite as: Vikrum Malhotra, Avni Thakore. 2020. Healthcare Post-COVID-19: Transitioning Healthcare Delivery Models to a “New-Normal”. Health Management, Policy and Innovation (HMPI.org), Volume 5, Issue 1, special issue on COVID-19, September 2020Abstract
The COVID-19 pandemic has forced the healthcare industry to confront extraordinary challenges. Healthcare providers have endured shortages in medical supplies, protective equipment, and market instability. Nonetheless, amid the crisis, strong public health measures, physical distancing, and transitioning to online services has provided reassurance that the COVID-19 curve may be flattening as the number of new cases has decreased and the number of patients that are hospitalized has stabilized.
These challenges and changes have ushered in a new era for the healthcare industry, including the transition to hybrid in-person and digital health practice models. As we continue to move toward the transition of healthcare from pre- to post-COVID-19, certain provisions can ensure the safety, efficiency, and effectiveness in healthcare delivery models. This article describes key changes in operations, communication, and security that are central to moving ahead effectively, including designation of specialty care facilities, creating emergency management plans, changing appointment policies, coordinating social distancing, managing hygiene protocols, and expanding testing.
Operations, Communication, and Security
Designation of Specialty Care Facilities
Governments should participate in a coordinated and effective method of hospital utilization by considering the designation of select hospitals as COVID-19-only specialty care facilities. These facilities will ensure properly trained staff, adequate PPE, expertise in treating complex patients, and proper ICU capacity (including negative pressure rooms when needed) for patients. This allows other hospitals to continue ongoing services to non-COVID-19 patients with active medical conditions without risking transmission and contamination. Governments should also utilize their resources to plan for the management of outbreaks in vulnerable populations and locations.
Emergency Management Plans and Teams
Healthcare practices should maintain emergency management plans that outline practice operations and the impacts on healthcare providers and patients that coronavirus may have. These plans can include pandemic coordinators, risk communications, essential functions, delegations of authority, continuity of facilities and communications, human resources, essential records management, testing and training, and reconstitution planning. They may choose to implement shift work for multispecialty office practices with providers staggered over the course of a day to reduce waiting room crowding and infection risk.
Consideration should also be given to assembling physician-staff teams so that monitoring the spread of coronavirus is attainable and practices may continue to operate in the event of positive results within a team. Clinic staffing must be structured to limit exposure and mitigate risk in the event a staff member gets sick as contact tracing and active testing become the new norm.
Practices should have continued access to communication that can be established by testing remote access to servers and email systems or the use of secure and cost-effective cloud options if access is restricted. Information should be kept within HIPAA regulations to ensure the security of sensitive data. Practices should also have access to critical information such as updates from CDC on COVID-19 for healthcare professionals.
Appointment Policies
Providers should institute a protocol for telemedicine to reduce the risk of transmission. Telemedicine appointments can include chronic care management, primary care, mental health, post-hospital discharge follow-up and post-op follow-up, thereby allowing providers and patients to maintain the practice of physical distancing while still providing timely, efficient and effective continuity of care. Patients can also utilize online payment methods via patient portals for billing and co-pays if needed. Providers should emphasize that non-urgent care can be obtained through telemedicine or rescheduled for a later time following local and state guidelines.
Nonetheless, offices should remain open for emergent needs or those requiring management in-office. Appropriate spacing of in-person appointments must be made to reduce wait times in the waiting room and allow for efficient evaluation of patients. On arrival, patients should have options to self check-in via a tablet service to reduce crowding. Patients needing to visit a practice can also be checked-in by phone and advised to wait in the parking area until called in. Patients can also be screened via questionnaires and administered temperature checks before entering the practice to further reduce the risk of transmission.
Social Distancing
Continuing social distancing practices post-COVID is crucial to the operations of healthcare practices. Providers should only allow patients inside the practice, restricting family members, friends, and children from entering except in extenuating circumstances. If there is any reason that this restriction cannot be met, only one person should accompany the patient. Practices should place signs that discourage sitting in waiting areas and tape off distances of six feet per CDC guidelines.
Hygiene Protocols
Developing protocols for proper hand hygiene, PPE, and sanitation of equipment should be a priority for healthcare practices. Providers may require the use of hand sanitizer by all patients and visitors to the practice and increase postage of signs in restrooms for proper hand hygiene. To further protect staff and patients, the installation of “sneeze guards” should be implemented on all diagnostic equipment that requires close contact and proper protective wear should be made available to all physicians and staff. Practices should also initiate frequent, thorough disinfection of waiting areas, restrooms, exam rooms, administrative tools, and equipment.
Expanding COVID-19 Testing
As testing capabilities expand, appropriate use of diagnostic testing for COVID-19 — ideally at the point of care — should be incorporated into pre-admission testing requirements prior to surgery and invasive procedures. Timely screening of healthcare personnel with known exposure risk should also be implemented in human resources guidelines. As more knowledge is gleaned regarding antibody testing for potential immunity to COVID-19, this testing modality should be incorporated to position personnel at lower risk of infection appropriately in critical care environments.
Looking Forward
Government and healthcare collaborations will prove to be critical tools in the functioning of healthcare practices. Protocols geared toward operations, appointments, social distancing, and hygiene and workflows that incorporate advances in COVID-19 testing can help practices transition toward a “new normal” in the post-COVID era. These guidelines can help ensure the safety of patients, physicians, and healthcare personnel and allow for effective and efficient healthcare.
Dealing with Predictable Surprises from COVID-Related Operational Changes (8/4)
Stephen Lewis, MD, MHCDS, and Bryan Spear, MBA, MHA
Contact: Stephen.lewis1972@gmail.com
What is the message: Deliberate COVID planning must include thoughtful mitigation strategies for predictable surprises. Strategies include understanding capacity and demand, as well as engaging with stakeholders to understand delivery gaps and reopening challenges. What is the evidence? The authors draw upon their experience at relevant medical centers. Timeline: Submitted June 8, 2020; accepted after revisions: August 3, 2020 Cite as: Stephen Lewis, Bryan Spear. 2020. Dealing with Predictable Surprises from COVID-Related Operational Changes. Health Management, Policy and Innovation (HMPI.org), Volume 5, Issue 1, special issue on COVID-19, August 2020Abstract
Predictable Surprises
Max Bazerman and Michael Watkins [1] defined the term predictable surprise as the disasters that organizations should see coming. They note organizations routinely fail to take one or more of three key steps in avoiding predictable surprises: recognition, prioritization, and mobilization.
The COVID-19 novel corona virus – and especially the follow up to it — is a predictable surprise. The pandemic abruptly changed healthcare operations as health system leaders prepared for possible hotspots in COVID-19 demand surges. These operational reprioritizations, new social distancing requirements, uncertainties, and significant fear surrounding the virus led to abrupt stoppage in the delivery of a significant proportion of routine healthcare. The pace of change in healthcare delivery also required relatively decentralized decision making, with clinics and services individually determining cancellation, rescheduling, and staffing policies, as well as telehealth practices.
While the pressure from a growing queue of patients eased with the expansion of telehealth, not all patients’ needs can be addressed virtually. Many patients who have specific needs regarding diagnostic testing or chronic condition management face increased acuity. This presents a unique, but predictable, problem when considering planning for the return to “new normal” healthcare delivery operations.
A Framework to View the Problem
As organizations consider approaches to re-expand direct patient care inside of a new and evolving paradigm for healthcare delivery, key externalities can be easily recognized. Based on the accumulation of patients with delayed care, providers can expect the acuity level of some patients to rise due to a lack of treatment. The figure below depicts a phenomenon in which, while the hospital begins to reopen fully, the system will be stressed beyond its available resources even after the COVID specific patient surge passes.
There are two main elements to understanding this problem.
- Capacity: First is the capacity of the healthcare system post COVID surge. As local restrictions ease, staff will seek and deserve time off to personally recover from the COVID surge which will lower the overall capacity of some services.
- Demand challenges: Second, there will be a rapid demand increase, above the rolling 12-month average, of interdependent services such as referrals, diagnostics, and administrative support. This is attributable to patients with above average acuity re-entering the system first. These patients’ complexity, exacerbated by breaks in continuity of care, may drive above-average requirements for diagnostic testing, referrals, and care management.
These two elements — post-surge decreased staffing capacity plus increased demand — create a predictable surprise for the many hospitals seeking a path forward towards resuming normal operations.
Gathering Data for Solutions
To address this utilization risk, healthcare systems should start at the clinic and service level to understand how they delivered care during the first several weeks of the COVID-19 crisis. It is important to prioritize understanding patient risk stratification approaches, medical service interdependencies, and how virtual health was implemented.
We recognize that only specialists can appropriately risk-stratify their patients. Discussions with these providers suggested global population risk assessment and prioritization was less familiar to specialists. Our observations also indicated significant heterogeneity across the organization in how virtual health was operationalized.
Solving the problem at each institution requires two types of information from key stakeholders within an organization.
- Delivery gaps: First, to capture variation and associated healthcare delivery gaps, senior leaders can send each front-line leader a comprehensive survey with three main sections: Access to Care, Continuity of Care, and Virtual Health.
- Reopening: Second, senior leaders should also present front-line leaders with a series of questions to prepare for reopening, again with three main topics: Staff Reintegration and Capacity Planning; Clinic Operations; and Physical Space Preparation.
The goal is to pair this information with centrally gathered utilization data to tailor operational recovery plans to specific clinic and service needs while creating an integrated global plan.
Looking Forward
Reflecting on our core mission to provide safe, timely, and effective care, we are all preparing to prevent a predictable utilization surprise associated with rapid and variable healthcare delivery operational changes. We should seek a comprehensive coordinated solution built upon customized local solutions that address specific clinical and service differences.
References
[1] Bazerman, M. H., & Watkins, M. (2004). Predictable surprises : the disasters you should have seen coming, and how to prevent them. Boston: Harvard Business School Press.