Özden Engin Çakıcı, American University Kogod School of Business, and Alex F. Mills, Baruch College Zicklin School of Business
Contact: Ozden Cakici <cakici@american.edu
Abstract
What is the message? Telehealth pay-parity laws and regulations require payers to cover and reimburse certain healthcare services provided remotely to the same extent as if those services were delivered in a traditional office setting. COVID-19 has spurred additional proposed and enacted legislation aimed at ensuring telehealth pay parity. The primary argument for telehealth pay parity is that it promotes access to care and also provides better health outcomes for certain illnesses; but research shows that patients seeking acute care via telehealth may be more likely to require a duplicate visit. Several open questions remain regarding the business impact of telehealth pay-parity policies and the future of telemedicine in healthcare practices.
What is the evidence? The findings are based on a review of the literature in health policy, medicine, business operations, and recent proposed laws and regulations in the United States.
Timeline: Submitted: April 6, 2022; Accepted after review: September 21, 2022.
Cite as: Özden Engin Çakıcı, Alex F. Mills. 2022. Telehealth Pay Parity: The Current Debate and Insights from Business Research. Health Management, Policy and Innovation (www.HMPI.org), Volume 7, Issue 3.
What Is Telehealth and How Effective Is It?
Telehealth or telemedicine refers to the provision of healthcare services via any remote platform, i.e., any service where the patient is not physically present with the healthcare provider. The advancement of technology has enabled many clinical services to be provided seamlessly via telehealth, while other services may be more challenging to perform in a telehealth environment. The challenges surrounding telehealth have traditionally meant that insurance coverage for telehealth services has been limited.1
The U.S. Department of Health and Human Services states that “telehealth treatment options are vast, but they vary depending on the condition and the patient’s needs and abilities”.2
To illustrate a case where telehealth can seamlessly replace or even augment an office visit, consider a patient who has diabetes, a chronic illness. This patient can measure her own blood sugar level at home using an electronic blood sugar meter, and automatically upload those measurements to her endocrinologist’s practice. In this case, telehealth may help the provider monitor this patient’s condition more frequently without the patient needing to repeatedly travel to a doctor’s office. Using a remote clinical service may improve the patient’s health outcome and, in return, may reduce overall healthcare spending by preventing patients from getting worse and requiring more expensive emergency services.
To illustrate a case where telehealth may be less effective at providing clinical services, consider a patient with a suspicious mole on her skin, who wishes to be examined by a dermatologist. Although the dermatologist can visually examine the mole via a video visit, the doctor may conclude that they cannot diagnose whether the patient’s mole is benign or malignant without a biopsy. This patient needs a subsequent office visit to receive additional clinical services for an accurate diagnosis. Therefore, choosing telehealth for this service is inefficient, because it requires two visits to the physician (one via telehealth and one in the office) where a single office visit would have sufficed.
The potential for variation in effectiveness of telehealth for different types of clinical services naturally leads to questions about how services provided by telehealth should be reimbursed, which is the focus of the remainder of this article.
What Is “Telehealth Pay Parity” and Why Does It Matter?
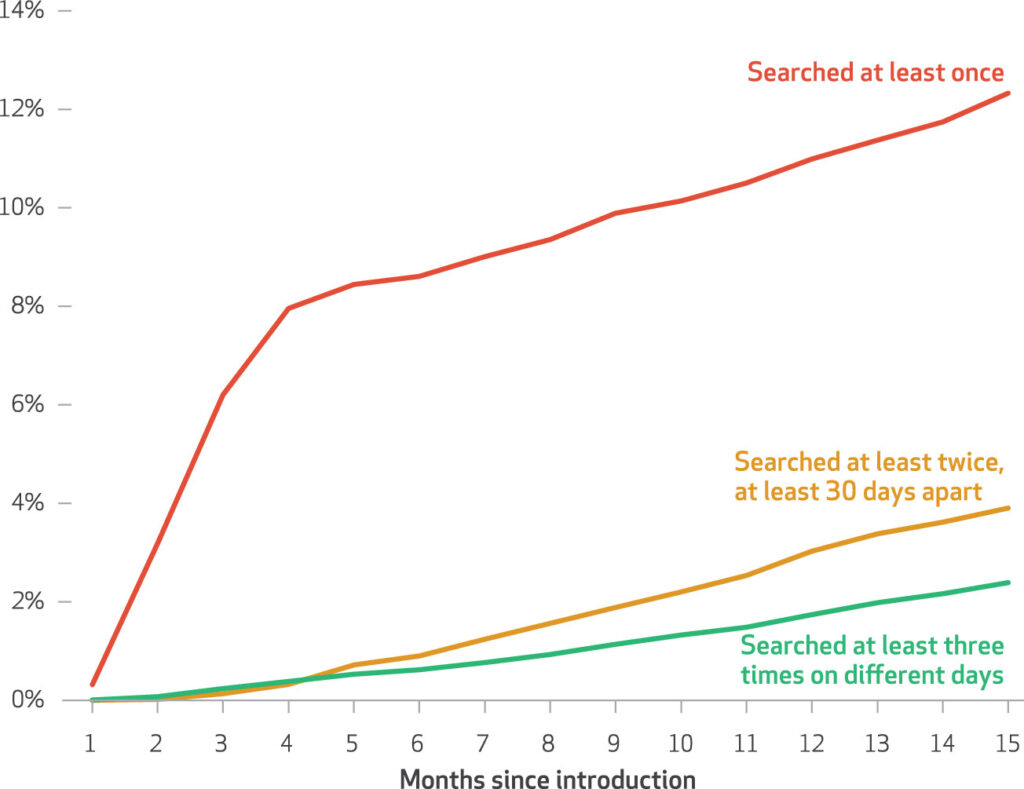
Telehealth has traditionally been reimbursed in a limited fashion, mainly for certain chronic illnesses and for patients in rural areas3. With the onset of COVID-19, awareness and acceptance of telehealth has increased, especially for acute care patients. Prior to the COVID-19 pandemic, fewer than 2% of clinicians provided any outpatient care via telemedicine. In the wake of COVID-19-related stay-at-home orders, providers had no choice but to switch many of their clinical services from traditional office visits to telehealth. There was a subsequent 23-fold increase in telemedicine from January to June 2020, spanning the specialties of medicine.4
As a result of this increased usage of telehealth, providers started to push more to get telehealth covered by insurance plans and to receive payment at parity with a traditional office visit. While physician offices have since largely reopened, healthcare provider organizations such as the American Medical Association and the American Hospital Association have started actively supporting the position that payers should not differentiate between telehealth and in-person services when reimbursing providers.5 Policies aimed at eliminating such differentiation are known as telehealth pay-parity policies.6 Although these policies differ by jurisdiction, they generally require that payers cover a service via telehealth if it would have been covered in the office, and provide equal payment for a clinical service, regardless of whether it was delivered via telehealth or in a physician’s office.7
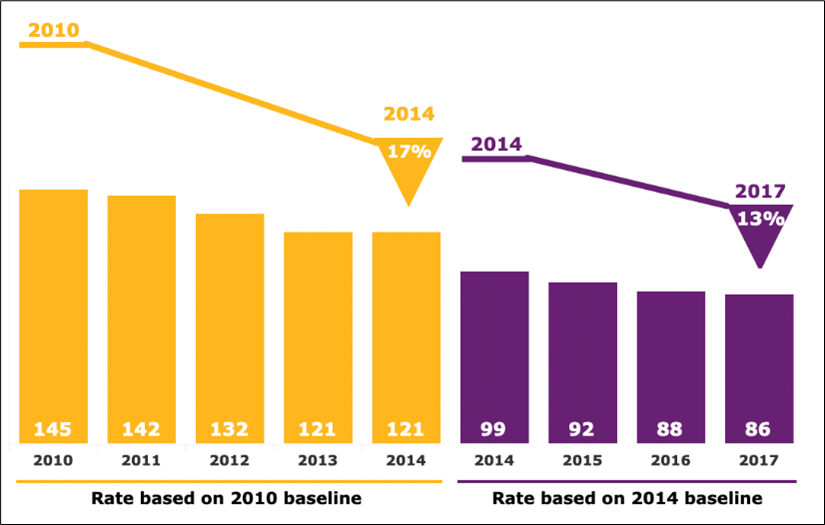
Numerous telehealth pay-parity policies were introduced during the COVID-19 pandemic. State telehealth pay-parity statutes more than doubled from 2019 to 20227. The U.S. Centers for Medicare and Medicaid Services (CMS) enacted a temporary telehealth pay-parity policy for Medicare recipients in March 20208, and bipartisan legislation under consideration in the 117th U.S. Congress would make that policy permanent9.
How Does Telehealth Pay Parity Fit into the Debate about Healthcare Reimbursement in the U.S.?
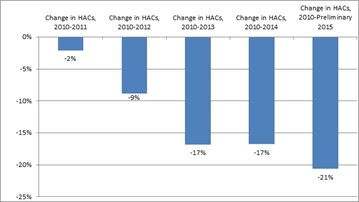
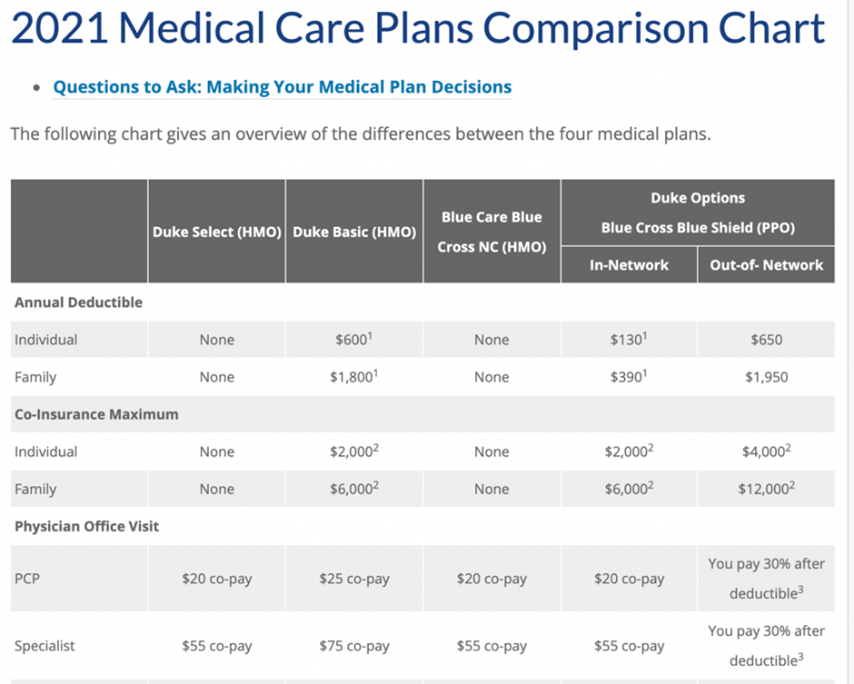
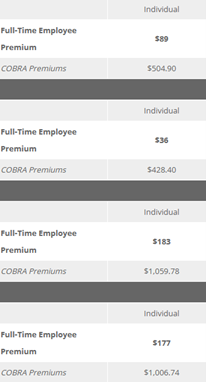
In the U.S., there are two main reimbursement models for healthcare services: fee-for-service and value-based payment.10 In the fee-for-service model, each service that a provider performs is reimbursed, hence “quantity” of care is the key determinant of provider revenue.11 On the other hand, value-based payment models reward quality of care. Examples of value-based payment include capitation, bundled payment, and pay for performance. In capitation, the healthcare provider is reimbursed a fixed amount per year per patient regardless of how many services the patient receives. Bundled payment is the reimbursement of health care providers based on expected costs for episodes of care. Under pay-for-performance payment, health care providers are offered financial incentives to meet certain health outcomes, and are penalized for poor health outcomes as well as medical errors and higher-than-expected costs.12
Fee-for-service is still the main reimbursement model for physician services in the U.S. healthcare system and is the main target for telehealth pay-parity policies. This means that for conditions where telehealth may not be as effective as an office visit, patients using telehealth might use an increased amount of healthcare services (for example, a telehealth visit and an office visit, where they previously would have had their problem resolved in a single office visit). This clearly has the potential to increase costs because healthcare providers are reimbursed separately for each visit. Note that this concern is distinct from the concern about “induced demand,” i.e., that the convenience of telehealth would induce patients to use more healthcare services or to use healthcare services more frequently. Even at the same level of demand, if telehealth is not as effective as a traditional office visit, it could still result in increased healthcare usage and costs.
Under value-based payment, particularly for pay-for performance, the effectiveness of telehealth is less of a concern because inefficient care is less likely to generate additional healthcare costs. However, the types of services that are reimbursed through value-based payment in the U.S. are typically hospital services (e.g., surgeries), which are unlikely to be feasible to conduct via telehealth.
What is the Case for Telehealth Coverage and Telehealth Pay Parity?
Two primary arguments in favor of telehealth coverage and telehealth pay parity are access and fairness.13 Seema Verma, the head of the U.S. Centers for Medicare and Medicaid services from 2017-2021, stated that “telehealth serves as an additional access point for patients” and that CMS-enacted telehealth pay parity during the COVID-19 pandemic “to make these services as widely available as possible.”14 Provider groups that support pay parity echo this theme of access, and, like Verma, they emphasize the advantages of telehealth for patients who are immobile15 or in rural areas where traveling to a healthcare provider may be burdensome.5,14 Thus, covering telehealth (particularly at pay parity) makes the healthcare system more fair for patients who might otherwise be disadvantaged, by enabling them to see otherwise-inaccessible providers. At the same time, providing telehealth is not necessarily a lower-cost alternative for providers, particularly those whose operational model is optimized for in-person visits. For example, a time-based study found that telemedicine actually incurred an incremental cost to the provider compared to an in-office visit.16 This strengthens the case that telehealth pay parity is necessary to ensure access because providers might not be willing to take on these disadvantaged patients for less than full reimbursement.
It is clear that telehealth pay parity provides an incentive for providers to offer telehealth, thereby increasing the overall availability of telehealth services14. What is less clear is whether the availability of telehealth itself increases overall access to healthcare, as patients could access care through multiple other channels, such as a hospital, a traditional office visit, urgent care, or a health clinic located in a retail pharmacy. Asserting that telehealth pay parity improves access to healthcare therefore relies on the premise that the availability of telehealth improves overall access to care. One piece of evidence that telehealth may increase access to care is found in commercial claims data. An analysis of claims found that 88% – of telehealth visits represented new utilization (i.e., they did not directly replace visits to other providers), and that this increased usage resulted in an overall increase in healthcare costs17.
What Is the Case against Telehealth Pay Parity?
Telehealth pay parity faces natural opposition from libertarian and free-market political organizations like the John Locke Foundation, who argue that telehealth has been thriving even without pay-parity laws, and therefore they prefer not to impose pay parity as an additional regulation18. They further cite “overconsumption” as a potential problem induced by telehealth pay parity. In other words, by making telehealth more widely available and accessible, inappropriate usage may increase.
Other think tanks have taken a more balanced stance based on cost-benefit analysis. For example, the Commonwealth Fund recommends that telehealth payments should be limited to services for selected patient populations and health conditions, or to services from providers that are paid via alternative payment methods.10
We do not find much credence in the position that adding a regulation regarding pay parity is itself a heavy burden on payers or providers. We also do not find this “induced demand” argument to be a credible reason to oppose telehealth pay parity because the same incentives that would increase inappropriate usage (reduced frictions for things like scheduling, transportation, and so on) also would increase appropriate usage. Indeed, the study of claims data that found telehealth leading to additional utilization could not identify whether that increased usage was appropriate or inappropriate.
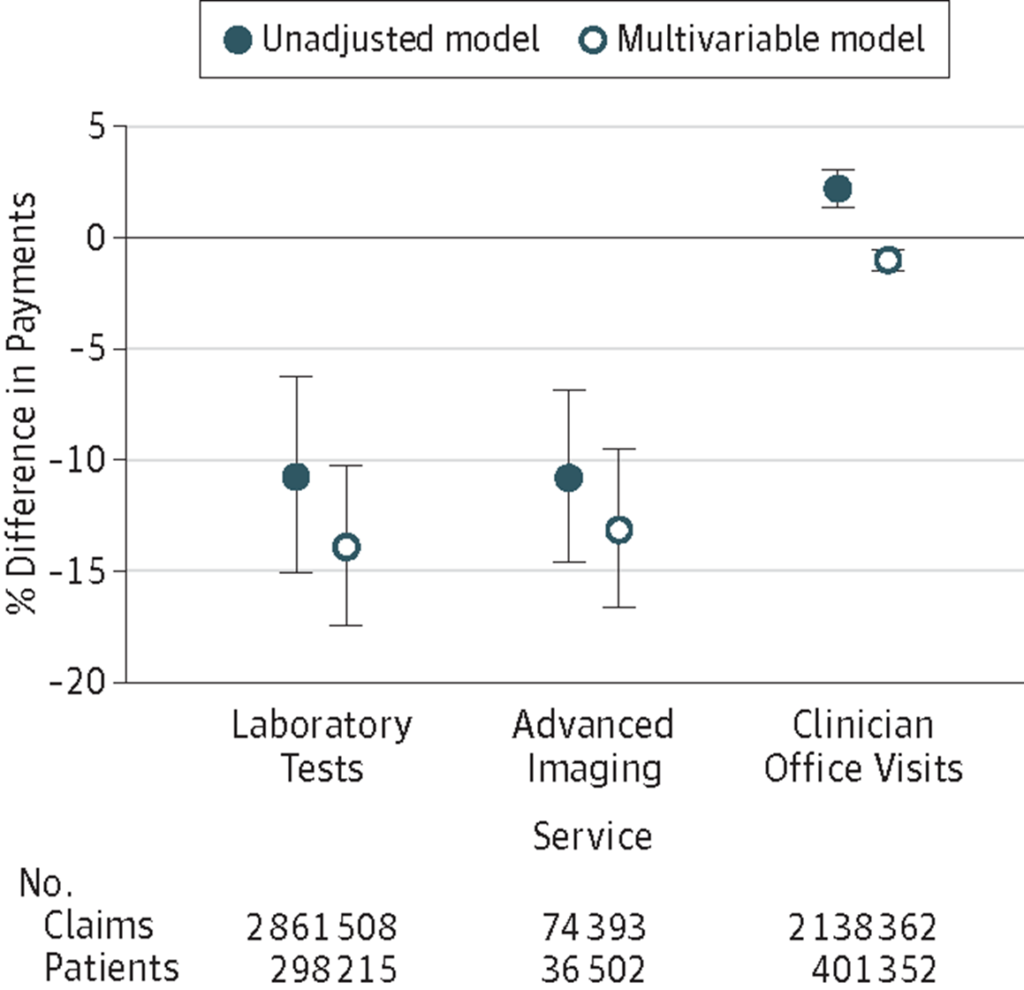
On the other hand, a salient argument against telehealth pay parity lies in its effectiveness. There is evidence that telehealth may not be as effective as in-person healthcare services, and consequently it may be a bad idea to pay providers equally for a less-effective alternative. A telehealth visit may be more likely to generate a subsequent in-person visit. A recent study suggests that differentially higher in-person follow-up visits after telemedicine (by phone and/or video) are consistent with pre-pandemic findings in direct-to-consumer telemedicine settings19. Also, telehealth visits are more likely to result in a routine 14-day follow-up visits20. All other things being equal, it would be better to resolve a patient’s health concern in fewer visits because in the fee-for-service environment, each additional visit represents increased healthcare costs for the payer, while in the value-based payment environment, each additional visit represents an investment of time and effort that is not separately reimbursed and thus is costly for the provider.
Several studies analyzing healthcare claims data indeed found that the rate of follow-up visits was significantly higher among patients whose first visit was via telehealth.3,21,22 For example, one study found 20% of patients receiving dermatology care required an in-person visit for reasons such as conducting a biopsy, which clearly cannot be done remotely.22 In other words, in 20% of cases, the dermatologist was paid for two visits, when one visit would have sufficed if the original visit had been in the office. These so-called “duplicate visits” represent an increase in healthcare spending without any corresponding improvement in outcomes. This increase in spending must be weighed against the consumer savings for the 80% of people who were able to avoid the time and expense of going to a doctor’s office. Hence, the costs and benefits should be analyzed for particular settings and specialties before concluding that telehealth pay parity would be the best possible reimbursement policy. When considering the effectiveness of telehealth, one may argue that traditional office visits may also have varying effectiveness but by and large, studies show that duplicate visit rates for telehealth are at least as high as that of traditional official visits, if not higher19, particularly for telehealth services that are marketed directly to consumers23. Verma, who implemented the Medicare pay-parity policy in March 2020, acknowledged the effectiveness concern, particularly around patients with acute healthcare concerns, stating that additional research was needed to assess outcomes7.
What Insights Does Business Research Offer?
While studies analyzing claims data point to an increase in access and utilization, coupled with a potential decrease in quality or effectiveness (for some specialties where duplicate visits may be more likely following telehealth than following a traditional office visit), they do not always attempt to understand the mechanism behind these impacts. Business research in the areas of operations management and decision sciences can provide insights into how patients access care and how policies such as telehealth pay parity may impact the business environment where care is delivered.
Healthcare providers act strategically when making choices about how patients should access care. In offering the decision of which access channels to offer, providers are generally motivated to obtain good health outcomes but also by financial remuneration. For instance, a healthcare provider may be interested in seamlessly delivering care across two access channels, in-person and telehealth, a practice known as omnichannel service delivery. While omnichannel service delivery is becoming more common in healthcare24, it has mostly been studied in other service contexts, such as retailing25,26 and restaurants27. But, a provider that traditionally offered all of their services in an office would have optimized their resources (e.g., personnel, supplies, equipment) for in-person care based on the demand for these services.28 Changing the delivery system to offer omnichannel healthcare by adding telehealth may lead to increased costs, coupled with the loss of revenue through shifting demand from in-person care to telehealth services, if pay parity is not enacted. The cost of bringing telehealth to the already optimized in-person care may outweigh its benefits in the short run16. So, in the short run it seems that pay parity might be a good incentive for providers to adopt telehealth.
However, payment parity may over-incentivize telehealth in the long-run after resources have been re-optimized, particularly in a fee-for-service system where the incentive is to provide as many “services” as possible. If providers are successful at driving down the unit cost of telehealth services (increasing their profitability), it might lead providers to shift too many resources to telehealth, neglecting the in-person channel. This kind of incentive-alignment problem becomes even more muddy when introducing value-based payment models, which further shift incentives. Rigorous business research that compares the operational costs and benefits of introducing telehealth under different reimbursement models is required.
Several published studies (not all of which directly study telehealth) provide some initial insight into this dilemma. Of particular interest is research showing that like providers, patients also act strategically when making choices about how to access care. Although patients are motivated to obtain good health outcomes, they are also motivated by convenience. When patients have a choice from among multiple types of providers (such as an urgent care, emergency department, or primary-care physician), providers’ managerial decisions influence patients’ subsequent decisions on where to access care29,30. Patients particularly consider trade-offs based on waiting time to get an appointment, anticipated in-clinic waiting time, time of the appointment, and preferred provider (e.g., if their primary doctor is available or not).31 These studies support the idea that by making healthcare more accessible through telehealth, patients may be more likely to seek healthcare.
For acute care, patients may arrive at a provider via scheduled appointments or without an appointment (i.e., “walk-ins”). A patient’s decision about whether to pursue an appointment or walk-in depends on the perceived convenience of each alternative, including wait times32. Incentivized by telehealth pay parity, providers may adopt telehealth by re-allocating some of the existing healthcare capacity that was previously devoted to scheduled appointments or walk-ins. Dividing existing capacity among additional channels may lead to increased wait times at the existing channels. The overall impact on patient access to acute care is therefore unclear, because most studies of telehealth neglect to consider the impact to existing channels.
Finally, a recent study shows that the adoption of telehealth for patients with chronic conditions not only results in more office visits, but it results in physicians accepting fewer new patients33. One reason for this may be that the convenience of telehealth allows providers and patients to see each other more frequently34, but more frequent visits for existing patients consume the provider’s time, which leaves less time available for new patients. As such, these studies suggest that telehealth pay parity could paradoxically decrease access to primary care by erecting barriers for access for new patients.
What is the Outlook?
Telehealth pay parity will continue to be a major policy debate through the years 2022-23. Business research suggests that policymakers should study the impact of telehealth on strategic and operational decisions of providers under different reimbursement models, which affect access. Understanding the difference in quality and convenience between a telehealth visit and a traditional office visit is also key to formulating a coherent policy, because the quality and availability of telehealth influences not only direct clinical outcomes, but also operational challenges like duplicate visits in acute care, and panel sizes in chronic care. Considering these, the business researchers should study (1) which specialties can be covered effectively via telehealth compared to a traditional office visit and (2) which reimbursement model would benefit the healthcare system if telehealth were also chosen as another access channel for healthcare delivery. The results would show a list of illness types that can be covered via telehealth and hence can be offered as an extra access channel to care. Given the mixed evidence on effectiveness of telehealth versus a traditional office visit, the overall economic impact of telehealth on providers and payers deserves further research. As telehealth becomes more widely adopted, state-level policies may be less influential as providers look to the federal government for guidance35. Policy decisions governing telehealth should therefore account for both the current state and the trajectory of health technology, patient and provider behavior, and preferences, the operational impact of changing incentives and reimbursement models.
References
- Chaet D, Clearfield R, Sabin JE, Skimming K, on behalf of the Council on Ethical and Judicial Affairs American Medical Association. Ethical practice in Telehealth and Telemedicine. J Gen Intern Med. 2017;32(10):1136-1140. doi:10.1007/s11606-017-4082-2
- Managing chronic conditions through telehealth | Telehealth.HHS.gov. Accessed September 14, 2022. https://telehealth.hhs.gov/providers/telehealth-for-chronic-conditions/managing-chronic-conditions-through-telehealth/
- Koma, Wyatt, Cubanski J, Neuman T. Medicare and Telehealth: Coverage and Use During the COVID-19 Pandemic and Options for the Future. KFF Issue Brief. Published May 19, 2021. Accessed September 14, 2022. https://www.kff.org/medicare/issue-brief/medicare-and-telehealth-coverage-and-use-during-the-covid-19-pandemic-and-options-for-the-future/
- Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation In Telemedicine Use And Outpatient Care During The COVID-19 Pandemic In The United States. Health Aff (Millwood). 2021;40(2):349-358. doi:10.1377/hlthaff.2020.01786
- Felt-Lisk S, others. Maintaining Flexible Telehealth Policies After COVID-19. Mathematica Policy Research; 2020.
- Haque SN. Telehealth Beyond COVID-19. Psychiatr Serv. 2020;72(1):100-103. doi:10.1176/appi.ps.202000368
- National Academy for State Health Policy. States Provide Payment Parity for Telehealth and In-Person Care. Published online 2021. https://bit.ly/3shGdR4
- Centers for Medicare & Medicaid Services. Medicare telemedicine health care provider fact sheet. Published online 2020. https://go.cms.gov/3Ht6bWg
- Phillips D. Telehealth Coverage and Payment Parity Act. Published July 16, 2021. Accessed December 6, 2021. https://www.congress.gov/bill/117th-congress/house-bill/4480/titles
- Porter ME, Kaplan RS. How to Pay for Health Care. Harv Bus Rev. Published online July 1, 2016. Accessed September 14, 2022. https://hbr.org/2016/07/how-to-pay-for-health-care
- Fee for Service – Glossary. HealthCare.gov. Accessed September 14, 2022. https://www.healthcare.gov/glossary/fee-for-service
- CMS’ Value-Based Programs | CMS. Accessed September 14, 2022. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs
- Ross C. I can’t imagine going back: Medicare leader calls for expanded telehealth access after Covid-19. STAT News. 2020;9. https://www.statnews.com/2020/06/09/seema-verma-telehealth-access-covid19/
- Verma S. Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19. Health Aff Forefr. Published online July 15, 2020. Accessed April 1, 2022. https://www.healthaffairs.org/do/10.1377/forefront.20200715.454789/full/
- Mills EC, Savage E, Lieder J, Chiu ES. Telemedicine and the COVID-19 Pandemic: Are We Ready to Go Live? Adv Skin Wound Care. 2020;33(8):410-417. doi:10.1097/01.ASW.0000669916.01793.93
- Ravitz N, MBA, Looby S, et al. The economics of a telehealth visit: A time-based study at Penn Medicine. hfma. Accessed September 14, 2022. https://www.hfma.org/topics/financial-sustainability/article/the-economics-of-a-telehealth-visit–a-time-based-study-at-penn-.html
- Ashwood JS, Mehrotra A, Cowling D, Uscher-Pines L. Direct-To-Consumer Telehealth May Increase Access To Care But Does Not Decrease Spending. Health Aff (Millwood). 2017;36(3):485-491. doi:10.1377/hlthaff.2016.1130
- Restrepo K. The Case against Telemedicine Parity Laws. Raleigh, NC: John Locke Foundation; 2018.
- Reed M, Huang J, Graetz I, Muelly E, Millman A, Lee C. Treatment and Follow-up Care Associated With Patient-Scheduled Primary Care Telemedicine and In-Person Visits in a Large Integrated Health System. JAMA Netw Open. 2021;4(11):e2132793. doi:10.1001/jamanetworkopen.2021.32793
- Phillips JC, Lord RW, Davis SW, Burton AA, Kirk JK. Comparing telehealth to traditional office visits for patient management in the COVID-19 pandemic: A cross-sectional study in a respiratory assessment clinic. J Telemed Telecare. Published online February 1, 2021:1357633X21990197. doi:10.1177/1357633X21990197
- Rabbani N, Chen JH. National Trends in Pediatric Ambulatory Telehealth Utilization and Follow-Up Care. Telemed J E-Health Off J Am Telemed Assoc. Published online May 11, 2022. doi:10.1089/tmj.2022.0137
- Uscher-Pines L, Malsberger R, Burgette L, Mulcahy A, Mehrotra A. Effect of teledermatology on access to dermatology care among Medicaid enrollees. JAMA Dermatol. 2016;152(8):905-912.
- Li KY, Zhu Z, Ng S, Ellimoottil C. Direct-To-Consumer Telemedicine Visits For Acute Respiratory Infections Linked To More Downstream Visits. Health Aff (Millwood). 2021;40(4):596-602. doi:10.1377/hlthaff.2020.01741
- Roth J. Omnichannel care delivery is becoming the next chapter of healthcare delivery. Microsoft Industry Blogs. Published September 28, 2021. Accessed September 14, 2022. https://cloudblogs.microsoft.com/industry-blog/health/2021/09/28/omnichannel-care-delivery-is-becoming-the-next-chapter-of-healthcare-delivery/
- Gao F, Su X. Omnichannel Retail Operations with Buy-Online-and-Pick-up-in-Store. Manag Sci. 2017;63(8):2478-2492. doi:10.1287/mnsc.2016.2473
- Gao F, Su X. Omnichannel Service Operations with Online and Offline Self-Order Technologies. Manag Sci. 2018;64(8):3595-3608.
- Feldman P, Frazelle AE, Swinney R. Managing Relationships Between Restaurants and Food Delivery Platforms: Conflict, Contracts, and Coordination. Manag Sci. Published online March 28, 2022. doi:10.1287/mnsc.2022.4390
- Bravo F, Braun M, Farias V, et al. Optimization-driven framework to understand health care network costs and resource allocation. Health Care Manag Sci. 2021;24(3):640-660. doi:10.1007/s10729-021-09565-1
- Cakici OE, Dewan R, Freimer M. Patient Choice in Acute Care. In: Proceedings of the 50th Hawaii International Conference on System Sciences. ; 2017.
- Sharma S, Xu Y, Gupta MK, Courcoubetis C. Non-urgent Visits and Emergency Department Congestion: Patients’ Choice and Incentive Mechanisms. Available SSRN 3480940. Published online 2019.
- Liu N, Finkelstein S, Kruk M, Rosenthal D. When waiting to see a doctor is less irritating: Understanding patient preferences and choice behavior in appointment scheduling. Manag Sci. 2018;64(5):1975-1996.
- Liu N, van Jaarsveld W, Wang S, Xiao G. Managing Outpatient Service with Strategic Walk-ins. Published online July 5, 2022. doi:10.2139/ssrn.3558209
- Bavafa H, Savin S, Terwiesch C. Customizing Primary Care Delivery Using E-Visits. Prod Oper Manag. 2021;30(11):4306-4327.
- Bavafa H, Hitt LM, Terwiesch C. The Impact of E-Visits on Visit Frequencies and Patient Health: Evidence from Primary Care. Manag Sci. 2018;64(12):5461-5480. doi:10.1287/mnsc.2017.2900
- Gaziel-Yablowitz M, Bates DW, Levine DM. Telehealth in US hospitals: State-level reimbursement policies no longer influence adoption rates. Int J Med Inf. 2021;153:104540. doi:10.1016/j.ijmedinf.2021.104540