Andrea Prado, Associate Professor, INCAE Business School; Priscilla Rodríguez, MBA, Senior Researcher, INCAE Business School; Alvaro Salas, MD, Professor, University of Costa Rica, Former President, Caja Costarricense de Seguro Social
Contact: Andrea Prado andrea.prado@incae.edu
Abstract
What is the message?
This case explores the key antecedents and development of the Costa Rican primary health model.
What is the evidence?
Costa Rican health indicators are comparable to those in OECD countries. A life expectancy of 79.9 years and a primary-level coverage of more than 90 percent can be used to demonstrate the success of the country’s primary healthcare model.
Submitted: October 2, 2019; accepted after review October 23, 2019.
Cite as: Andrea Prado, Priscilla Rodríguez, Alvaro Salas. 2019. Innovation in the Public Sector: The Costa Rican Primary Healthcare Model. Health Management Policy and Innovation, Volume 4, Issue 2.
Overview
The Caja Costarricense de Seguro Social (CCSS) is the most important healthcare provider in Costa Rica. In 2019, it received the United Nations Public Service Award for the implementation of its digital medical records, known as EDUS, in 100 percent of its facilities.2 EDUS is the latest in a series of healthcare innovations—many of them at the organizational level—encouraged by the Costa Rican government. Organizational innovations, often more than technological improvements, are responsible for dramatic cost reductions and value creation.3 Thus, scholars are strongly promoting health policies that encourage various types of organizational innovations.4
This case reviews the Costa Rican public healthcare system, particularly its innovative primary health care model that was launched in 1994. We discuss key antecedents and public policy decisions that allowed the EBAIS (Equipos de Atención Básica en Salud) model to become a successful organizational innovation.5,6 We analyze this model’s financial structure, as well as some of its main outcomes to date. The paper concludes by identifying takeaways for achieving high-quality universal health coverage, established as a priority among the United Nations Sustainable Development Goals for 2030.
The Evolution of Healthcare in Costa Rica
Current status
Costa Rica is a small country in Central America (51,100 sq. km) with a 2018 population of approximately five million. The country has a strong democratic tradition and abolished its army in 1948. Although Costa Rica is a middle-income country (about $16,900 GDP per capita in 2019), its social outcomes are comparable to those in high-income countries.1 For instance, Costa Rica has the second-highest life expectancy (79.9 years) in the Western Hemisphere—even longer than in the USA7. Maternal mortality (27 per 100,000 live births) and infant mortality (7.6 per 1,000 live births) rates are low compared to other Latin American countries and have been consistently decreasing for more than two decades.7
The country has broad-based access to healthcare services. In 2018, over 93 percent of the population had access to primary healthcare. It ranked high on the Healthcare Access and Quality index compared to nearby countries8 and was in the top ten percent in effective primary healthcare coverage among low- and middle-income countries. By 2019, even Costa Ricans in the lowest income quintiles could access full medical services at very low cost.9 The country achieved these results despite spending less on healthcare—per capita and as a percentage of GDP—than the world average.7
Only a few decades ago, Costa Rica exhibited poor health indicators. As recently as 1970, the infant mortality rate was 61.5 per 1,000 live births, and life expectancy was 65 years.10 The road to improvement needed to overcome barriers arising from economic conditions, both international and national, as well as political opposition from multiple interest groups.
Despite the challenges, the country achieved strong improvements, starting in the 1970s and continuing through the 1980s. In 1978, Costa Rica was praised at the Alma-Ata Declaration meeting for its achievements in primary healthcare. The Ministry of Health and the CCSS carried out policies that promoted organizational innovation. These polices, which were implemented consistently by multiple government parties through different time periods, led to health indicators comparable to those in developed countries.
Historical initiatives: 1920s to 1970s
The Ministry and Caja have long histories. The Ministry of Health was founded in 1922 with the responsibility for public health and provision of basic primary healthcare.11 The CCSS, was founded in 1941 to provide health and pension benefits to manual laborers and white-collar workers living in urban areas.
The evolving role of the CCSS is particularly important. The agency started with no services of its own, so outsourced them to the hospitals owned by the Junta de Protección Social, the national lottery organization that financed the Ministry of Health. At that time, only a small part of the population had access to health care, and the poor rural areas were badly neglected. During the first two to three decades after its creation, the CCSS was in a consolidation period as it sought to address this major gap. While it was attempting to extend its coverage to spouses and dependent children, the CCSS faced numerous challenges, including resistance by interest groups such as medical associations as well as political turbulence arising from the birth of the social democratic movement and armed intervention in 1948.10,12
The 1970s then provided a base of strong political commitment through two governments led by the social democratic party. This period was marked by a strong public investment in health, reaching seven percent of GDP.10 In 1973, the CCSS assumed control over the facilities of the Ministry of Health, including first-line health service establishments that provided users with their first contact points for healthcare. In doing so, the CCSS became the sole delivery institution of public hospital care, with 29 facilities around the country.13
The Ministry of Health, by contrast, focused on primary healthcare, including prevention of disease and promotion of health, now emphasizing rural areas and marginal communities. This transformation of the Ministry of Health as the leader in community health programs during the 1970s provided the building blocks of the country’s primary healthcare model developed in the 1990s. Moreover, some public health leaders consider this organizational innovation in Costa Rica as an antecedent of the policy that the World Health Organization (WHO) promoted worldwide, known as “Health for All by 2000.”10
Community health programs during the 1960s and 1970s
Several programs launched in the 1960s provided a basis for these improvements in health access in rural communities. Even before the 1960s, the Rockefeller Foundation supported efforts to implement community health programs, including antiparasitic and antimalarial campaigns. In addition, mobile assistance units and Health and Development Committees led by community members were financed by the Alliance for Progress, an initiative of U.S. President John F. Kennedy to promote economic, political, and social development in Latin America during the 1960s.10
Mobile assistance units in Costa Rica consisted of teams—a doctor, a nurse auxiliary, a sanitary inspector, and a driver—that visited rural towns on a monthly basis and provided free health consultations and educational talks to the inhabitants. Before leaving town, the doctor would meet with the community’s Health and Development Committee for a discussion of conditions that affected the residents’ health, such as water quality, waste and excrement management, and access to roads. Some of these discussions led to improvements. For instance, some communities organized to build an aqueduct as a result of these meetings. Health indicators showed a clear improvement during this initiative, and the Ministry gathered valuable household census data from the field visits. However, the program was short-lived; the mobile assistance units declined when international funding dried up.
The antimalarial program, by contrast, lasted longer and reached greater scale. The program expanded across the country during the 1960s. Then, due to its success in eradicating malaria, the program ended at the beginning of the 1970s.
The end of the antimalarial program left time availability among Ministry employees, who had been responsible for applying the pesticide dicophane (DDT) throughout the country. Despite strong resistance from health professionals in multiple institutions, the Ministry converted these workers into community health promoters by training them to deliver preventive health actions.10 For instance, both doctors’ and nurses’ professional colleges strongly opposed this proposal, arguing that only their trained members should be entitled to provide health services. Politically, however, the supporters of this proposal viewed it as a key complement to broad-based Social Security programs.
A financing law approved in 1974 that charged a five-percent tax on all payrolls allowed the government to massively extend the rural and community health programs. As much as 60 percent of the revenues generated were assigned to social initiatives such as child nutrition programs, clean drinking water, social housing, and immunization campaigns.
For instance, the Ministry created the CEN (Centros de Educación y Nutrición), CINAI (Centros Infantiles de Nutrición y Atención Integral) and CENCE (Centros de Educación y Nutrición y Comedor Escolar), a network of facilities that offered child care and protection services for children under age 13, for eight to 12 hours per day. In these facilities, children and pregnant women received free food and education. The Ministry delivered its health services through two types of centers: sanitary units around the country focused on parasitosis and maternal care, while health posts were small stations served by communitarian health assistants; there were no medical professionals at these posts. The assistants’ main duties were to provide preventive medicine and health education in communities with fewer than 2,000 inhabitants.10 Ill patients who arrived at health posts with complex diseases were referred to health centers for treatment. These centers belonged to the CCSS and offered their services through doctors, medical auxiliaries, nurses, and other professionals, such as dentists.
Daniel Oduber, the country’s president from 1974 to 1978, would say regarding government social investment: “Where health goes, everything else follows.” The rural health program’s coverage increased from 11 percent of the rural population with 50 health posts at the start of the program in 1973 to 60 percent with 301 posts in 1983.10
The gains during the 1970s were highly visible. Participants in the World Health Organization International Conference on Primary Health Care in September 1978 praised the Costa Rican rural and communitarian program. The Costa Rican representatives at the conference shared data showing that the country had achieved two years earlier (i.e., 1976) the goals that WHO had proposed for all members to reach by year 2000.14 The Ministry’s efforts through this program, as well as the legal restructuring to extend the coverage—outside of urban areas and to the non-working population—had resulted in the universalization of the health system. It was an exceptional achievement.10 By the end of the 1970s, in the entire western hemisphere, only Canada and Cuba had achieved the goal of universal health services.
Crisis: Mid-1970s to mid-1980s
Most of the social initiatives coordinated by the Ministry of Health and responsible for the results in terms of health indicators were financed by payroll taxes. In the late 1970s and early 1980s, Costa Rica found itself in an economic crisis generated by three main forces. First, a world crisis at that time had its largest effect on poor countries. Second, a new government came into power, with no clear vision or leadership for the health sector. Third, a neoliberal ideology took hold in the country.10 The net effect of these factors was that the Ministry discontinued its efforts to strengthen the rural and community health program, due mainly to budgetary limitations. The program’s annual budget went from 9.5 percent of GDP in 1976 to a 2.4 percent in 1986.10 The cutbacks in the program resulted in low public satisfaction and reduced quality of care.
The CCSS also faced one of its worst crises in the late 1970s and early 1980s. In 1979, it exhibited its first deficit. Between 1978 and 1982, despite maintaining the same infrastructure, the CCSS hired 40 percent more personnel. The growth in employment increased the financial deficit, even as the CCSS continued to offer essentially the same services. The losses led to the creation of the country’s Development Plan for 1982-1986. This plan emphasized the need to consolidate a National Health System that avoided duplicate efforts by the Ministry of Health and the CCSS. As a result, substantial improvements took hold over the next decade.
From dividing to combining responsibilities: Late 1980s and early 1990s
By the end of the 1980s, the division of responsibilities seemed to be working. The CCSS focused mainly on curative care and rehabilitation, while the Ministry focused on prevention of disease and promotion of health. Even with the Ministry and CCSS focusing on different aspects of healthcare, important challenges remained. There was still duplication in the processes and inefficiencies within and between the institutions. In addition, pressure from international organizations pointed towards reducing the size of public employment, such as the Ministry’s payroll. Thus, in 1994, Costa Rica undertook a major reform of its healthcare system by transferring the responsibilities of the Ministry to the CCSS.
The CCSS gained 2,325 new employees,6 creating challenges in dealing with bureaucratic integration processes and ideological differences across the combined agencies. Ministry officials had serious concerns about this move, arguing that public health was underrepresented in a more curative-oriented institution such as the CCSS. Nonetheless, creating the CCSS as an integrated agency that championed both public health and preventive services contributed to an organizational innovation in the form of a new primary health care model.
This primary healthcare innovation fit perfectly into the health sector reform during the 1990s. Two key pillars of the reform were emphasis on integrated care and strengthening the primary level of care. Integrated attention encompassed services that provide curative care, prevent disease, rehabilitate when necessary, and promote health through lifestyles and nutrition.15 By strengthening the primary level of care, the reform sought to modernize what had proven effective in the Ministry’s program: first contact with the user, thus opening the door into the system.15
Creation of the EBAIS: 1995 and into the 2000s
The reform involved a national movement to expand health coverage. The basis of the new primary health care model was the Equipos Básicos de Atención Integral en Salud, an organizational innovation consisting of health centers with multidisciplinary teams located across the entire country. The first EBAIS was launched 1995. Within ten years, Costa Rica had implemented a new national primary healthcare system.6
Differentiated teams
The EBAIS model is centered on the notion that prevention, promotion, curation, and rehabilitation are equally important. Each EBAIS had a multidisciplinary team consisting of at least one doctor, a nursing assistant, a technical assistant (asistente técnico de atención primaria, similar to a community health worker), a medical clerk (registros y estadísticas de la salud), and a pharmacist.6
Team members have differentiated tasks. Doctors deliver curative and preventive care, such as managing acute and chronic conditions, diagnosis and treatment. Nurses are responsible for basic clinical tasks and health counseling. The pharmacist prescribes medication. The technical assistant engages in health promotion and disease prevention activities; inspection of basic housing conditions and sanitation, epidemiological data collection, identification of environmental and familial behavioral risk factors and referrals to EBAIS or hospitals.6 Unlike the physicians and nurses, the technical assistant conducts her activities outside of the clinics, either through individual home visits or group visits in community settings such as schools, churches, and town centers.6 Finally, the medical clerk takes charge of records and statistics at the facility and is responsible for patient intake, collecting and managing patient data, and epidemiological population health surveillance.6
The CCSS assigns households to an EBAIS through a strategic geographic division of the territory, often referred to as empanelment or sectorization process. Each facility is meant to serve approximately 5,000 people. All households are geographically empaneled in the EBAIS model, which helps to explain its high coverage rate—reaching 94 percent of the population by 2018. The sectorization process has been key to expanding the coverage of primary healthcare throughout the country. Its success can be attributed to the fact that it went beyond assigning households to EBAIS on a map, as an office exercise. In the field, EBAIS teams had their assigned households clearly identified (e.g., location and socioeconomical profile of their members) and performed epidemiological surveillance through home visits. Thus, sectorization allowed the CCSS to effectively include households within the system, significantly increasing its health coverage.
Three benefits of EBAIS empanelment for users stand out: Users receive first-contact access, the ratio of patients to clinicians is manageable, and care is continuous.6 The technical assistants at the EBAIS are crucial in this process, as they visit households regularly and provide first-contact care for users. They record household data in a family file, including a risk score that determines the frequency of future home visits.6 Indeed, it is due the work of these technical assistants that the CCSS has been able gain access to each household served by a single EBAIS. By 2017, 1,042 EBAIS were providing primary-level care to the people of Costa Rica.16
System integration
EBAIS are integrated into a network structure with the rest of the health system, which includes general and specialized hospitals and clinics. If a patient needs specialized medical attention beyond primary care—not available at the EBAIS—the CCSS has 20 regional and peripheral hospitals that provide secondary care. These hospitals are spread across the country for geographic accessibility. Additionally, the CCSS has three general national hospitals in the capital city, which offer a third level of attention. The agency also has six specialized establishments concentrated in the central valley region that provide tertiary care.
This network structure embodies an integrated system. All national, specialized, and regional hospitals, plus the EBAIS, function as a network model that is articulated horizontally and vertically. With the multi-party integration, patients can navigate the network through a reference and counter-reference system and receive the attention required.16
Funding the EBAIS system
Costa Rica’s healthcare system aims for contributive solidarity, meaning broad-based financial support.11 CCSS health insurance is financed by a 15-percent payroll tax towards which employers, employees, and the government contribute 9.25 percent, 5.5 percent, and 0.25 percent respectively.5,17 All workers in the country, including the self-employed, are obligated to contribute.17 Contributions for unemployed people are covered by the government, drawing on taxes on luxury goods that are transferred to the CCSS to cover low-income families’ healthcare.18
Outcomes of the EBAIS reform
Achieving this universal primary healthcare system was challenging. Decisions such as merging the Ministry of Health with the CCSS and implementing the innovative EBAIS model required strong political will and commitment from the government. The decisions also required compromises from the institutions involved to facilitate the integration and allow the new model to consolidate.
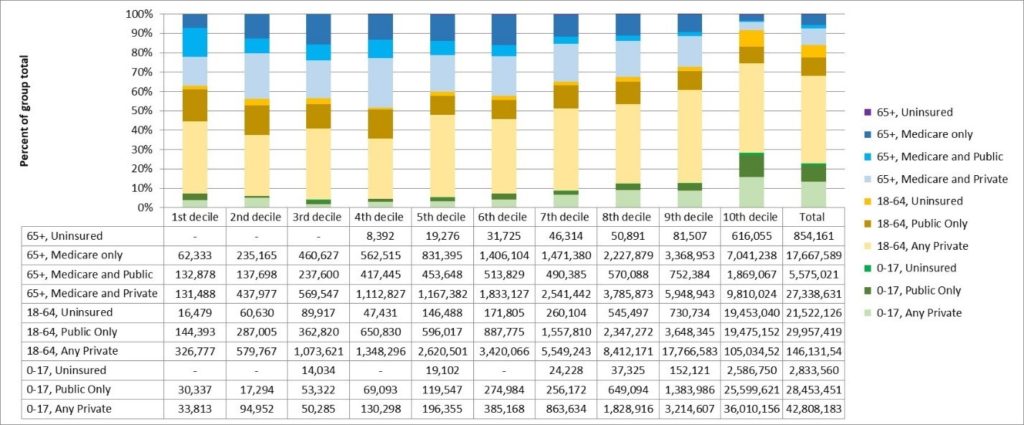
Nonetheless, looking back on the results obtained during the past five decades, the efforts led to broad-based healthcare services. By 2012, the lowest quintile of the population, who receive only 4.7 percent of national income, received nearly 30 percent of all health expenditures, while the wealthiest quintile, generating 48 percent of the national income, received 11 percent of CCSS resources.17 Hence, in addition to system solidarity in funding, those who are less privileged benefit most from the system.
Coverage statistics are striking. From 1995 to 2001, the number of EBAIS teams increased from zero to 736 clinics, covering 80 percent of the population.19 In 2017, over 93 percent of the population had access to primary healthcare.6
Health indicators improved significantly after the 1994 reform. As we reported earlier, life expectancy at birth increased in more than three years after 1995 to eventually reach 79.9 years in 2017, about the level of the OECD average of 80.2 years.7 Key indicators such as maternal mortality, infant mortality, and deaths from infectious diseases have also experienced continuous improvement since 1995.
Nonetheless, major challenges remain. Non-communicable chronic diseases are now the most common burden of disease among the Costa Rican population17 and are estimated to account for 83 percent of all deaths in the country.20 For instance, the incidence of deaths caused by ischemic heart disease and stroke increased by 63 percent and 78 percent, respectively, between 2007 and 2017.21 The EBAIS system offers a platform to address this challenge, by promoting preventive efforts, healthy lifestyles, and follow-up to chronic care services.
Lessons Learned
The consolidation of the Costa Rican primary healthcare system within the EBAIS, building on the history of Ministry of Health and CCSS initiatives, offers lessons for countries interested in strengthening their first level of attention to health and healthcare needs. In discussing lessons learned, it is important to emphasize that health is both a leadership and a political issue. None of these results would have been achieved without the commitment and determination of visionary leaders who constantly had to overcome strong resistance from multiple interest groups, including pressure from international organizations to follow the conventional wisdom of development approaches.
Three organizational features of the EBAIS model allowed it to consolidate and achieve its results. First is the multidisciplinary nature of the EBAIS teams that are trained to provide not only curative, but also preventive and promotional activities at the first point of contact with the system’s users. Such early contact reduces costs for the system, for example, by making early diagnoses and providing users with faster access to basic services. It is important that the EBAIS team reaches out to the assigned population through household visits and community events, rather than waiting for patients to come into the clinic. In addition, there is high value in having a team member in charge of the data collection and analysis, which provides inputs for decision-making and for monitoring the population’s needs.
Second, the geographic empanelment feature is crucial. Distributing primary care facilities so that all households are assigned to a facility allows the system to have a high coverage rate, thus providing access to services for almost all the population. Some countries have tried such community assignments, though typically not at the nationally-distributed level, with broad-based inclusion of rural areas. Other countries have empaneled households in a geographic area but more as a theoretical exercise than as an effective practice in the field. In this regard, the role played by the technical assistant in the EBAIS model is key to reaching out to community members by collecting their epidemiological and socioeconomic data and monitoring their condition, promoting healthy behaviors, and preventing diseases, among other things. Visiting individual homes or meeting households in community settings, instead of waiting for individuals to visit the EBAIS, often when they get sick, strengthens the effectiveness of the model’s empanelment feature.
Third, the network structure that combines hospital services with the primary level of care is critical. Without a reference and counter-reference system, EBAIS patients would not have access to more-complex treatments at the secondary or tertiary level. This distributed integration means that patients gain services both at the point of initial care and over the life cycle of their medical needs.
Certainly, providing high healthcare coverage generates challenges to the health system. For instance, ensuring that all citizens have first-care access has substantially increased the volume of referrals to secondary and third-level hospitals. In the last decade, long waiting times for specialized medical consultations or surgical procedures has negatively affected patient satisfaction and imposed administrative pressures on the institutions. As an example, more than 40 percent of patients in need of treatment for prostatic hyperplasia in 2017 had a waiting time greater than 366 days; for cataracts, this percentage was 30 percent. Thus, health systems seeking to strengthen their primary care systems also need to anticipate how patients can effectively navigate higher levels of medical care. Coordinating health institutions through an effective network approach constitutes a necessary organizational innovation to support strong primary care systems.
Looking ahead, the EBAIS model is now providing a platform to address current epidemiological challenges of non-communicable diseases. Critically, the EDUS digital records system can combine with the EBAIS, using household and individual data that are now available in a single medical record that can be accessed from anywhere in the system. The EBAIS and EDUS, working together, have the potential to create another powerful organizational innovation in the Costa Rican healthcare system.
References
1 Social Progress Imperative (2018). Social Progress Index. Retrieved September 16th, 2019, from https://www.socialprogress.org/
2 United Nations (2019, June 21). UN recognizes public institution-led initiatives in 11 countries that are advancing Sustainable Development Goals. Retrieved September 16th, 2019, from UN: https://www.un.org/development/desa/en/
3 Richman, B., Mitchell, W., & Schulman, K. (2013). Organizational Innovation in Health Care. Health Management, Policy and Innovation, 1(3):36-44.
4 Porter, M., Teisberg, E. (2006). Redefiningh Health Care: Creating Value-Based Competition on Results. Boston, Massachusetts.: Harvard Business School Press.
5 Cuccia, L., Chadwick, J., Hassam, A., Kim, A., Sivarajan, R., & Wong, V. (2019). Costa Rica’s Health Care Reform: Impact and Success of the EBAIS model. The Prognosis, 8(1):24-35.
6 Pesec, M., Ratcliffe, H., Karlage, A., Hirschhorn, L., Gawande, A., & Bitton, A. (2017). Primary Health Care That Works: The Costa Rican Experience. Health Affairs, 36(3):531-538.
7 World Bank Group (2019). Indicators. Retrieved September 16th, 2019, from World Bank: https://data.worldbank.org/indicator
8 GBD 2015 Healthcare Access & Quality Collaborators (2017). Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. The Lancet, 390:231-66
9 Caja Costarricense de Seguro Social (2018). Informe de Resultados de la Evaluación de la Prestación de Servicios de Salud 2017 [Results Report of the Evaluation of the Provision of Health Services 2017]. San José: Editorial Nacional de Salud y Seguridad Social.
10 Miranda, G. (1988). La Seguridad Social y el Desarrollo en Costa Rica [Social Security and Development in Costa Rica]. San José: Caja Costarricense de Seguro Social.
11 Vargas, J. R., & Muiser, J. (2013). Promoting universal financial protection: a policy analysis of universal health coverage. Health Research Policy and Systems, 11:28.
12 Homedes, N., & Ugalde, A. (2002). Privatización de los servicios de salud: Las experiencias de Chile y Costa Rica [Privatization of health services: The experience of Chile and Costa Rica]. Gaceta Sanitaria, 16:54-62.
13 Unger, J.P., De Paepe, P., Buitron, R., & Soors, W. (2008). Costa Rica: Achievements of a heterodox health policy. American Journal of Public Health, 98(4):636-643.
14 Morgan, L. (1990). International Politics and Primary Health Care in Costa Rica. Social Science & Medicine. 30(2):211-219.
15 Salas, A. (1998). Caja Costarricense de Seguro Social: Presente y Futuro [CCSS: Present and Future]. San José: Caja Costarricense de Seguro Social.
16 Caja Costarricense de Seguro Social (2018). Memoria Institucional 2017. San José: Caja Costarricense de Seguro Social.
17 Montenegro, F. (2013). Costa Rica Case Study: primary health care achievements and challenges within the framework of the social health insurance. Washington D.C.: The World Bank.
18 Cercone, J., & Pacheco Jiménez, J. (2008). Costa Rica Good Practice in expanding health care coverage. In W. Bank, Good Practices in Health Financing: Lessons from reforms in low- and middle-income countries (pp. 183-225). Washington D.C.: The World Bank.
19 Clark, M. (2002). Health Sector Reform in Costa Rica: Reinforcing a Public System. Washington D.C.: Wilson Center
20 World Health Organization (2016). Countries: Costa Rica. Retrieved September 26th, 2019, from WHO: http://www.who.int/nmh/countries/cri_en.pdf
21 Institute for Health Metrics and Evaluation (2017). Country Profile: Costa Rica. Retrieved September 26th, 2019, from https://www.healthdata.org/